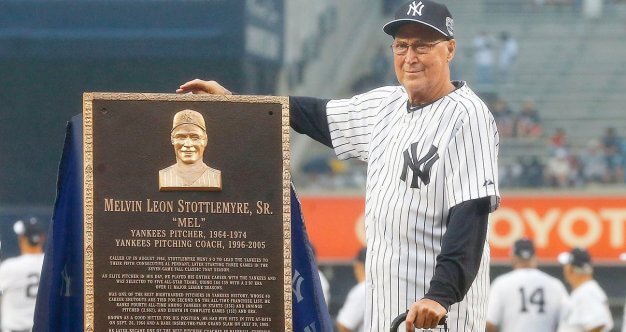
We’ve just learned that baseball legend Mel Stottlemyre passed away after many years dealing with multiple myeloma. Stottlemyre was a legend for anybody who cares about the New York Yankees. For a whole other community of multiple myeloma survivors, his longevity through the disease represents a watershed.
We can’t know everything about Stottlemyer’s disease, however, there has been an enormous amount of progress in the field of multiple myeloma. Ken Anderson, Director of the Jerome Lipper Multiple Myeloma Center at Dana Farber Cancer Institute and the Kraft Family professor of medicine at Harvard Medical School about some of the recent innovations in multiple myeloma, tells us , “There has just been a paradigm shift in the way we think about myeloma and the way we treat myeloma as a consequence in the way patients and their families can enjoy the much improved outcome. We actually treat patients earlier, before they develop complications like anemia, bone disease, high blood calcium, or kidney disfunction, therefore intervene early to prevent these complications.”
Read MoreDr. Nina Shah, a hematologist at UCSF, told us that myeloma can be one of the trickiest to diagnose– a diagnosis often starts with a patient telling their doctor they feel tired, weak, or have notices increases in the number of infections they get in a year. It also often starts with some pain in the back, hips or scull. After a diagnosis, a series of blood tests can help doctors understand protein levels, blood count, and your DNA. The DNA test help doctor’s determine levels of risk, which can help with treatment.
After myeloma treatment, recurrence is possible. Dr. Shah tells SurvivorNet that there are available resources for trying to keep myeloma at bay after treatment, including drugs that help keep the immune system on guard for the possibility of myeloma’s return.
Learn more about SurvivorNet's rigorous medical review process.