Advocating for Early Prevention of Ovarian Cancer
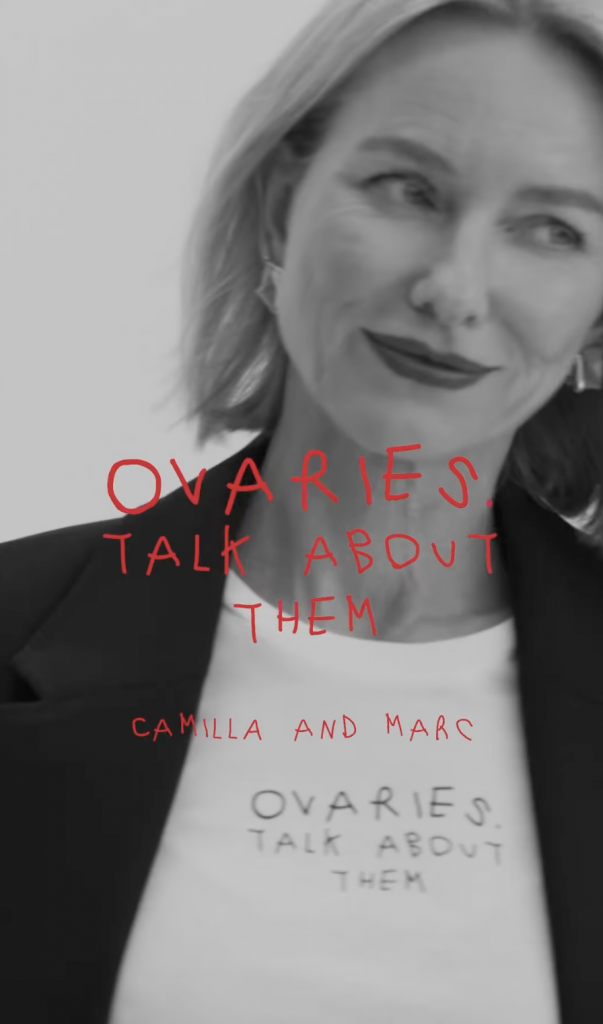
- Naomi Watts, 55, has joined fashion label Camilla and Marc’s 5th annual ovarian cancer prevention campaign, ‘Ovaries. Talk About Them,’ to raise awareness about a disease that is too often caught in a later stage.
- The campaign’s initiative is to help support the further development of an early detection test, which, as of now, there isn’t one available. However, the University of New South Wales in Australia, with its groundbreaking research, is getting close.
- One in five women have a hereditary predisposition of ovarian cancer, yet 80% of women with ovarian cancer are not getting a genetic test. If a woman is born with a BRCA1 or BRCA2 mutation, they have up to a 50 percent chance of developing ovarian cancer. Genetic testing also helps determine your treatment if you have been diagnosed with this disease.
- So, although there isn’t yet a reliable screening method, knowing your ovarian cancer risk can help you be more closely monitored, and your medical team can steer you to consider a preventative option, like a hysterectomy.
The luxury brand’s founders, siblings Camilla Freeman-Topper and Marc Freeman, lost their mother to ovarian cancer when she was 42 years old. They were just 13 and 11 at the time.
Read More
View this post on Instagram
“How much are your ovaries worth? The label’s Instagram site reads. “Over 310,000 women are diagnosed worldwide each year, with over 75% diagnosed in the late stages when it is often too late. An early detection test is desperately needed to save the lives of millions of women and people with ovaries around the world and to safeguard our future generations.”
Learning More About Ovarian Cancer
Despite ovarian cancer’s reputation for being a devastating disease, what most people don’t realize is that when it’s detected early enough, it has a better than 90% cure rate. The problem is, it’s not an easy disease to diagnose, especially in its early stages, so only 20% of cases are caught early.
It’s important to remember that there isn’t just one ovarian cancer; there are many different types that are more likely to occur at different life stages. In fact, researchers have identified more than 30 types, but these three are the most common:
Epithelial: Over 90% of ovarian cancers are epithelial, which means the cancer cells are located on the outer layer of the ovary. Most epithelial tumors are benign, but when they’re malignant, they’re not usually caught until the disease has advanced about 70% of the time.
Stromal: These are a rare class of tumor (only 3 5% of cases) which forms in the connective tissue that holds the ovary together and produces estrogen and progesterone.
Germ Cell: These tumors develop in the cells that produce the ova, and are more likely to impact a single ovary, rather than both. When you hear about a teen or young woman being diagnosed with ovarian cancer, it’s usually germ cell. The good news is, about 90% of these cases can not only be cured, but the woman’s fertility can also be preserved.

One thing that these types of cancer have in common is that they’re tricky to diagnose. Because the symptoms of ovarian cancer are non-specific and can be misattributed to anything from menopause to last night’s sketchy supper, most women don’t even mention their symptoms to their doctors until they become severe. And then there’s the lack of any widely available screening test for the disease.
Yearly pelvic exams and pap smears can screen for many different conditionsSTDs, pregnancy, various infections, along with gynecological cancers of the cervix, uterus, fallopian tube, and vulva. If your gynecologist includes a rectovaginal exam, they can check and see how the ovaries feel, but a pelvic exam alone is not an effective screening mechanism for this kind of cancer.
While we have mammograms to scan for breast cancer (though they’re not 100% accurate), colonoscopies which reveal anything suspicious lurking in the colon or rectum, and cervical cancer which can be diagnosed via a pap smear or HPV test, unless there’s a family history of ovarian cancer along with recurring symptoms, most gynecologists will not suggest an in-depth workup for the disease.
Dr. Beth Karlan, a gynecologic oncologist at UCLA Medical Center, says, “In certain high-risk women, who have either inherited a defect in a gene called BRCA1 or 2 or other associated genes with hereditary ovarian cancer, you should undergo an ultrasound of the pelvistrans-vaginal ultrasoundand a CA-125 [blood test], because it’s the best we have at the current time.”
Is There Screening for Ovarian Cancer?
But these tests are only routinely available for women with the aforementioned family histories of cancer, inherited genetic conditions such as Lynch syndrome and/or women presenting with recurring symptoms of the disease.
So while there’s no widespread screening method currently available, researchers (like the Australian scientists previously mentioned) are working hard to find one. As Dr. Karlan says, “finding an early detection method for ovarian cancer is really like the holy grail.”
Navigating an Ovarian Cancer Diagnosis
An ovarian cancer diagnosis can turn your world upside down. All of your priorities your family, your partner, your job — have to immediately shift to accommodate your cancer and its treatment. It’s no wonder that depression and anxiety are so common in ovarian cancer patients.
“It’s not unusual for me to have patients tell me that they are having extreme anxiety, sadness, changes in their mood, in coping with the disease diagnosis and getting through treatment,” Dr. Jayanthi Lea, gynecologic oncologist at the University of Texas Southwestern Medical Center in Dallas, Texas, previously told SurvivorNet.
Coping After Learning About Your Diagnosis
The first thing Dr. Lea asks her patients about is their diet and sleep habits. “Because very often, people stop eating. They can’t sleep,” she says. “And then the other component is, do they have somebody close to them that they can talk to — a spouse, a loved one, a friend? These are all important things, because it’s important for people to get some type of normalcy amidst the chaos of being told that they have an advanced stage ovarian cancer.”
If you feel overwhelmed by emotions right now, talk to a psychologist, psychiatrist, or other mental health professional. Also lean on the doctor who treats your cancer. “Patients should not forget that oncologists are very much a part of their team. We are on your side. So when you have spoken to your family members or your spouse and you still feel that you are having challenges in trying to just cope from day to day, come and talk with us,” Dr. Lea says.
Genetic Testing For Ovarian Cancer: Why Is It Important?
“We know that about 20%, and the numbers may be even higher, of our patients with ovarian cancer have a hereditary predisposition,” Dr. Jocelyn Chapman, a gynecologic oncologist at UCSF Medical Center, previous told SurvivorNet. Additionally Sheryl Walker, a cancer genetic counselor at Genome Medical in Dallas, Texas told us about 80% of women with ovarian cancer are not getting a genetic test.
Women who are genetically predisposed to ovarian cancer were likely born with genetic mutations in their DNA which increases their risk of developing the disease. Seeing as many women may not know they have these mutations, testing is important to not only identify whether a patient is at higher risk, but also determine the best course of treatment after a diagnosis.
“These genes don’t mean [women] will definitely get cancer, but to give an example, in the general population one in every seventy women will get an ovarian cancer diagnosis in their lifetime, [and] if you’re born with a BRCA1 or BRCA2 gene mutation those are the most frequently diagnosed gene mutations and your risk increases up to 50% so that would be a one out of two,” Dr. Chapman said.
Ovarian Cancer and Genetic Testing
Once receiving an ovarian cancer diagnosis, patients will be referred to a doctor for genetic testing to see if they have hereditary dispositions. By going through testing, doctors can determine different treatment strategies that will best suit a patient’s needs.
“This information now is crucially important to understanding what treatments [will] most benefit [patients],” Dr. Chapman added.
What Are BRCA1 And BRCA2?
BRCA1 and BRCA2 are proteins that work as tumor suppressors. They help repair damaged DNA, and are important for ensuring the stability of each cell’s genetic material. If either of these genes is altered, that mutation can mean that its protein product does not function properly, or that damaged DNA may not be repaired correctly.
BRCA1 and BRCA2 are traditionally associated with cancers specific to women, such as breast and ovarian, and are commonly passed down among family members. In fact, if one of your blood relatives is found to carry a BRCA gene mutation, there’s a 50-50 chance you could be carrying it, too. However, BRCA mutations aren’t found on the X or Y sex chromosome, so you’re just as likely to inherit the risks of cancers associated with BRCA from your father as you are from your mother. Plus, in the U.S., it is reported that 90 percent of people who carry a BRCA gene mutation aren’t aware that they’re carrying it until someone in their family gets cancer.
Identifying the BRCA mutation isn’t just about letting the patient’s family members know to be vigilant with screening, but there are new therapies available for ovarian cancer patients with BRCA mutations, as well as encouraging research being done to improve health outcomes. Even women with no familial history of ovarian cancer could have the BRCA1 or BRCA2 mutation genetically present. Whether that’s the result of their having small families (or a variety of other reasons), a lack of ovarian cancer diagnosis in the family is not a rational reason to forego being tested. Certain populations, such as Ashkenazi Jews and those with Mediterranean roots, are particularly susceptible to these mutations. Between the potential benefit to the family members and to the patient herself, it is important that patients understand the value in the genetic testing.
Contributing by SurvivorNet staff.
Learn more about SurvivorNet's rigorous medical review process.

