Empowering Yourself and Others Is Always Beautiful
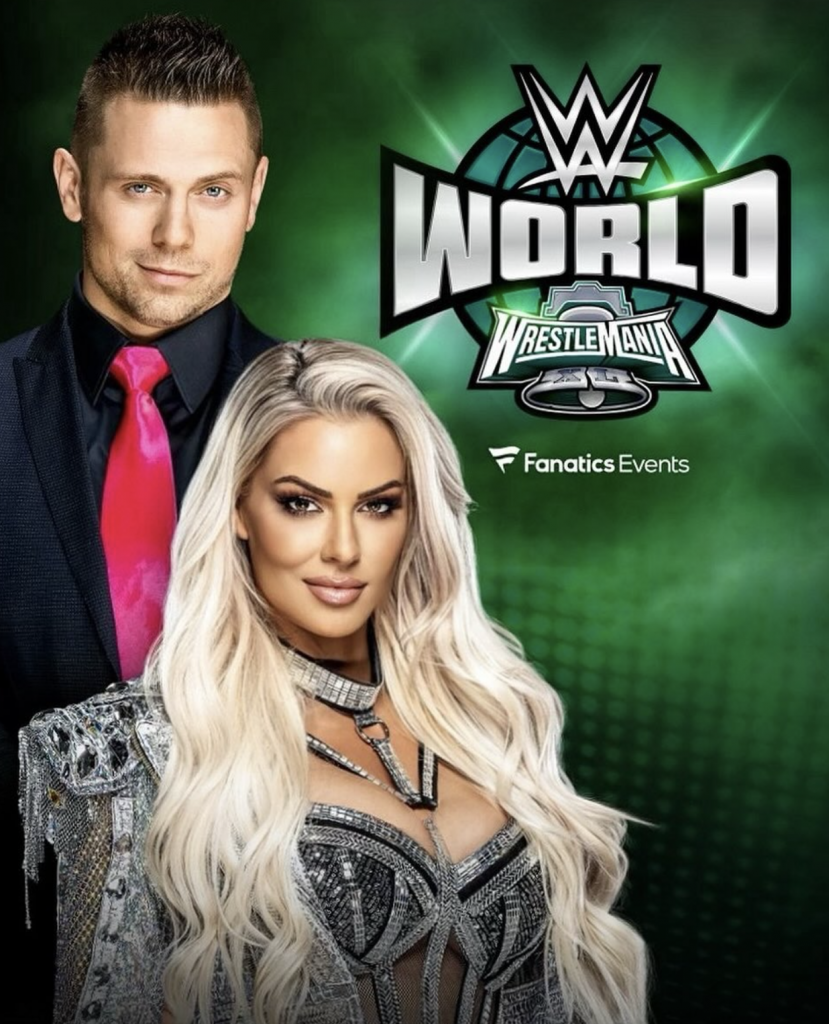
- WWE star Maryse Mizanin, 41, is not letting her post-surgery scars stop her from being proud of her body. The mom of two daughters had surgery to remove numerous pre-cancerous tumors around her ovaries back in February, candidly sharing her story to help encourage others to advocate for their health – and stay strong while doing it.
- Ahead of Fourth of July, the Canadian TV personality, 41, shared a stunning full-length post of herself posing in a red-white-and-blue American flag bikini, displaying her scars and urging people to feel empowered by their resilience, which was met by a flurry of praise and thanks for the inspirational post.
- Body image changes after cancer treatment (or preventative surgeries like Maryse) are very common. Many women consistently report struggling with side effects like scars or other physical changes that can come after surgery. Inspiring stories like SNTV’s Body Image: Embracing Your Body, a part of the original series SN & You, along with Maryse’s story, can help inspire you to learn to love your body again.
Ahead of Fourth of July, the Canadian TV personality, 41, shared a stunning full-length post of herself posing in a red-white-and-blue American flag bikini and sassy white platform heels, urging people to feel empowered by their resilience.
Read More
View this post on Instagram
After the share, Maryse’s comments section exploded with thanks and praise for her impactful message.
“You’re beautiful! I burned my stomach with a heating pad trying to relieve pain from endometriosis yesterday and I know it’ll go away but it looks so ugly right now and you just reminded me that little things like that don’t matter as long as we are healthy,” one fan wrote. “Beautiful inside outside and in the side!”
Another follower shared how much the image meant to her as a mother of a child going through something similar. “Thank you for posting this,” she said. “My 19 year old daughter had emergency surgery on Tuesday to remove a 14cm dermoid cyst on her right ovary, which they had to remove also. She was devastated after surgery from the laparoscopy incisions.”
“I told her about your journey and showed her your pictures. I hope she will see the beauty in her scars one day.”
A third woman expressed even more emotion: “I’m fighting back tears right now. You truly are a warrior. It takes great strength, courage and straight fire to show your vulnerable side,” she said. “I’m so glad you shared your journey and inspired so many other women to not be afraid to show your scars. They’re the mark of a true champion”
Maryse’s Health Story
In February, Maryse shared that she had been suffering from severe abdominal swelling to where she “looked six months pregnant.”
“Lots of GI issues,” she wrote, meaning gastrointestinal problems, “extreme fatigue” and “multiple rounds of antibiotics.”
She had flare-ups that came and went over the course of that past year, but then the pain became “chronic” and more and more difficult to manage.

Numerous scans and tests didn’t show anything wrong. Maryse had her allergies checked and even had her house inspected for mold.
After “countless” doctors, she finally met a “patient, attentive, and genuinely caring” woman, Dr. Thaïs Aliabadi (who is the reason actress Olivia Munn discovered her breast cancer after a “normal” mammogram), who “truly listened.”
Performing a minor surgery, Dr. Aliabadi discovered 11 “implants around my uterus, ovaries, and all connective tissues around the organs in my abdominal cavity,” Maryse wrote. They were serous borderline tumours, a “sneaky, aggressive,” rare pre-cancer of the ovaries.
Maryse went on to have a full hysterectomy, which is the removal of the uterus and cervix.

“Let’s bring light to a huge woman healthcare issue here,” she continued. “Women get so conditioned to believe that it is normal to suffer, most often in silence. Told to stop being a crybaby, that it must be hormonal imbalances, just anxiety or just all in your head. This is not normal. This cycle has to be broken!”
Concluding her compelling post, she added: “Advocate for yourself and keep pushing! Follow your instincts. Never underestimate your gut feelings.”
Pushing for a Correct Diagnosis
When it comes to your health, be a little pushy. You know your body better than anyone else. When you see a doctor for a problem, don’t hesitate to make sure that your question is fully answered and that you are comfortable with the plan moving forward. From a doctor’s perspective, every problem should have a diagnosis, a treatment, a plan for follow-up, and a plan for what happens next if the treatment doesn’t work.
As a patient, if you don’t feel like each of these four things has been accomplished, just ask. Even if it requires multiple visits or seeing additional providers for a second opinion, always be your own advocate.
Be Pushy, Be Your Own Advocate, Don’t Settle
Dr. Zuri Murrell, director of the Cedars-Sinai Colorectal Cancer Center, previously told SurvivorNet that healthcare guidelines are meant to do the right thing for the largest number of people while using the fewest resources.
“The truth is you have to be in tune with your body, and you realize that you are not the statistic,” he said.
Additionally, Dr. Murrell says not every patient will “fit into” the mold, so it’s important to “educate yourself and be your own health care advocate.”
“Every appointment you leave as a patient, there should be a plan for what the doc is going to do for you, and if that doesn’t work, what the next plan is,” Dr. Murrell added. “And I think that that’s totally fair. And me as a health professional that’s what I do for all of my patients.”
‘Body Image: Embracing Your Body’
As for the so-called aftermath, after a diagnosis and potential subsequent surgery, there are additional hurdles that you may go through and just know you are not alone.
In SurvivorNetTV’s Body Image: Embracing Your Body, a part of the original series SN & You, we follow the journeys of four women and their battles with breast cancer as they reconcile and learn to love their bodies again.
These women have been through everything including single mastectomies, double mastectomies, chemotherapy and radiation, but this episode shows how the power of the human spirit can triumph over self doubt and adversity.
Watch SNTV’s Empowering Story on Body Image
Body image changes after cancer treatment (or preventative surgeries like Maryse had) are very common. In fact, women going through breast cancer and ovarian cancer report struggling with side effects like scars or other physical changes that can come after surgery.
Watching this short film can help put these challenges into context and offer support from women who have been through similar situations.
Ovarian Cancer Prevention: Methods for High-Risks Patients
For high-risk women like Maryse, a number of exciting technologies have emerged in recent years that can help to prevent ovarian cancer.
Dr. Ritu Salani, a Gynecologic Oncologist at The Ohio State University, previously explained a number of strategies to SurvivorNet, which include genetic testing for susceptibility, surveillance methods that can aid early detection and medications that can reduce risk.
Dr. Salani broke down the ways in which the availability of genetic testing has changed and how doctors find women who are at risk for ovarian cancer.
“We are really excited about how genetic testing has really revolutionized ovarian cancer care,” Dr. Salani said. “When you have a relative who’s been affected with ovarian cancer or certain types of breast cancer, oftentimes genetic testing is performed.”

These tests focus in on the BRCA I and II genes, which usually fight against tumor growth in the body. Genetic tests can now determine whether mutations exist in these genes, which is a reliable sign of a woman having a genetic predisposition for ovarian cancer.
If these tests come back showing a genetic cause for the woman’s disease, then the rest of the woman’s family should be brought in. “If they test positive, then this would be important for their family members to be tested, because this is our best opportunity to prevent a cancer from developing,” Dr. Salani said.
“So, if a family member tests positive, usually the first and second members will be tested, and if they test positive then we’d have some opportunities.”
Once doctors can firmly establish the genetic susceptibility to ovarian cancer in a family, then they have several available paths to prevent the disease. One method that doctors have utilized to limited success is to surveil a woman’s levels of CA-125, a protein biomarker that is often more present in the blood of those who are at high risk for ovarian cancer. This test can be helpful, but there are also a number of reasons other than cancer that a patient’s CA-125 levels might be high.
Doctors can also perform transvaginal ultrasounds (TVUS). These tests utilize sound waves to get a visual of the uterus, fallopian tubes, and ovaries. While they can locate the presence of a mass, they cannot on their own determine whether a mass is malignant or benign. (CA-125 and pelvic ultrasounds are not recommended for use to screen asymptomatic women without established genetic risk factors for ovarian cancer.)
RELATED: Genetic Testing and Ovarian Cancer
Beyond these limited surveillance methods, doctors are increasingly using birth control pills as a means of ovarian cancer prevention. “One of the most exciting and probably understated medicines in the OBGYN world are birth control pills, or what we call oral contraceptives pills,” Dr. Saloni shared. Oral contraceptive pills (OCPs), which have been common forms of contraception for over half a century, can reduce risk for ovarian cancer by up to 50% if taken for five years.
The precise reasons why OCPs so decrease the likelihood of ovarian cancer are still obscure.
Dr. Salani states that OCPs can be effective for those both with BRCA mutations and for the general population. “And that’s not only true for ovarian cancer, it’s also true for endometrial or uterine cancer. So there’s a lot of promise in birth control pills.” Dr. Salani also reminds women, however, that there are risks in taking OCPS. “It’s not always safe for everybody,” she says. “So it’s important to understand what those risks are and if you’re a candidate for it. But it is one of the most powerful chemopreventive agents that we know of.”
Even with these advances, for those women who have BRCA mutations the safest form of prevention is still the removal of the fallopian tubes and ovaries. This removal is recommended for women who show a BRCA I and mutation by age 35 to 40.
Dr. Saloni talked through the difficulties of this decision for women. “We know that these are important instruments in childbirth and if you’re young and you still haven’t completed your family, then this is not something that would be appropriate for you.”
Even if removal is not feasible, however, surveillance and OCPs can still be a remarkably effective method for many high-risk individuals to prevent ovarian cancer.
Contributing by SurvivorNet staff.
Learn more about SurvivorNet's rigorous medical review process.


