Living With Advanced Thyroid Cancer
Resources, expertise, and survivor support to help you after a diagnosis
When you’re facing advanced thyroid cancer, having trusted guidance can make all the difference. That’s why our team at SurvivorNet, after countless conversations with both patients and renowned thyroid specialists created Living With Advanced Thyroid Cancer – a comprehensive guide to support you through every step of your journey.
Drawing on our extensive reporting and the firsthand experiences of our community, this resource goes beyond clinical information to address the real challenges you may face during treatment and beyond.
Facing Thyroid Cancer
Facing Thyroid Cancer: An Overview
After getting an advanced thyroid cancer diagnosis, it can be challenging to sift through all of the new information you are getting — and to focus on the tasks ahead, like finding a doctor, deciding where to get treatment, and weighing the pros and cons of each treatment option.
It’s important to understand that even in advanced stages, there are still good treatment options for thyroid cancer. If you are still in the process of putting together a treatment team and plan, we’ve gathered some guidance from experts to help you with these next steps.
“The message I try to impart is that it is possible to live a very healthy, productive, and active life after a diagnosis of thyroid cancer,” Dr. Lisa Orloff of Stanford Cancer Center told SurvivorNet. “It should not have an impact on life expectancy if it’s treated properly in the early phases.”
Even highly respected doctors sometimes disagree about a diagnosis and believe patients should embark on different treatment paths — that’s why you shouldn’t be afraid to seek a second opinion if you want to.
National Cancer Institute Chief of Surgery Steven Rosenberg recommends seeking out multiple professional opinions to confirm a diagnosis and figure out the options.
Dr. Lisa Orloff of Stanford Cancer Center explains, “It’s really important to undergo thorough evaluation and treatment planning before rushing to a decision about treatment. I think it’s okay to take time, meaning sometimes several months to navigate the healthcare system and obtain preferably more than one opinion about management.”
Dr. Orloff also recommends connecting with an endocrinologist in addition to otolaryngologist to arm yourself with advice from different perspectives. This will allow you and your care team to create an optimal individualized treatment plan.
There are also perks to seeking care at a cancer center where multiple specialists come together to discuss a patient’s diagnosis and care plan.
This may help you make key treatment decisions.
+ Expand and Learn More About Comprehensive Cancer Centers ...
Not everybody can get to a designated comprehensive cancer center, but the data is clear that these centers are extremely helpful — especially when your disease is complex and advanced.
There are plenty of excellent physicians who are not at comprehensive cancer centers. That being said, when you are looking into care, you should be asking, “Am I getting doctors with different specialties like medical oncology, radiation oncology, surgery, pathology and radiology?”
The really important thing is that you have a team that is up to date with the latest science. That can happen away from a major cancer center or it can happen at one. In order to get the best guidance, it’s important to get comfortable asking your doctor questions and bringing up your concerns.
What Your Thyroid Does
Understanding the Thyroid Gland
“Our thyroid gland is a butterfly shaped endocrine gland that sits in front of our windpipe. We think of it as kind of our energy driver. Its main purpose is to produce thyroid hormone,” Stephanie Giparas, a physician assistant at the Endocrine and Head and Neck Department at Moffitt Cancer Center, tells SurvivorNet.
“The thyroid hormone not only regulates our metabolism, but almost every organ system in our body uses thyroid hormone. It supports our heart, it supports our brain. So you cannot live without thyroid hormone.”
Your thyroid plays a vital role in regulating numerous essential bodily functions, from metabolism to heart rate. If your treatment plan includes a thyroidectomy—complete removal of the thyroid gland—you’ll need daily thyroid hormone replacement medication. These medications effectively take over the crucial functions your natural thyroid once performed.
+ Expand and Learn More On Thyroid Function & Cancer Risk ...
The thyroid is responsible for several functions throughout our body, including:
- Metabolism: The thyroid produces hormones — mainly thyroxine (T4) and triiodothyronine (T3) — that influence how fast your body uses energy (your “metabolic rate”).
- Heart Rate and Blood Pressure: These hormones help control how quickly your heart beats, which can also affect blood pressure.
- Body Temperature: By affecting the speed at which your cells operate, thyroid hormones play a part in regulating body temperature.
- Other Functions: The thyroid also works closely with the pituitary gland in your brain. This gland makes thyroid-stimulating hormone (TSH), which signals the thyroid to release more or fewer hormones based on your body’s needs.
It’s important to know that having an overactive or underactive thyroid does not necessarily increase the chance of developing thyroid cancer. Many people experience hyperthyroidism (when the thyroid produces too many hormones) or hypothyroidism (when the thyroid does not produce enough hormones) without ever developing cancer but these conditions should be treated to correct the hormonal imbalance they represent.
Cancer risk factors include:
- Exposure to Radiation: Head or neck radiation treatments during childhood, or exposure to higher radiation levels (for example, nuclear accidents), can increase risk.
- Family History: Certain genetic conditions (especially affecting the RET gene) can raise the likelihood of developing some types of thyroid cancer.
- Iodine Deficiency: The thyroid uses iodine to make hormones, so low iodine intake can sometimes be linked to certain thyroid problems. However, because salt is often iodized in many countries, this is less common in places like the U.S.
- Gender and Age: Thyroid cancer is three times more likely in women. It is frequently found in women in midlife and men in later years.
Thyroid Cancer Types
Types of Thyroid Cancer
Thyroid cancers are classified by their cellular origin, which directly influences their behavior, prognosis, and treatment approach. In our conversations with leading endocrine oncologists across institutions like Memorial Sloan Kettering Cancer Center and Fred Hutch Cancer Center, we’ve learned that understanding your specific type is crucial for making informed decisions.
Differentiated Thyroid Cancers
“Differentiated” means that the cancer cells still look somewhat like normal thyroid tissue under the microscope. These typically start in follicular cells, the part of the thyroid responsible for making hormones.
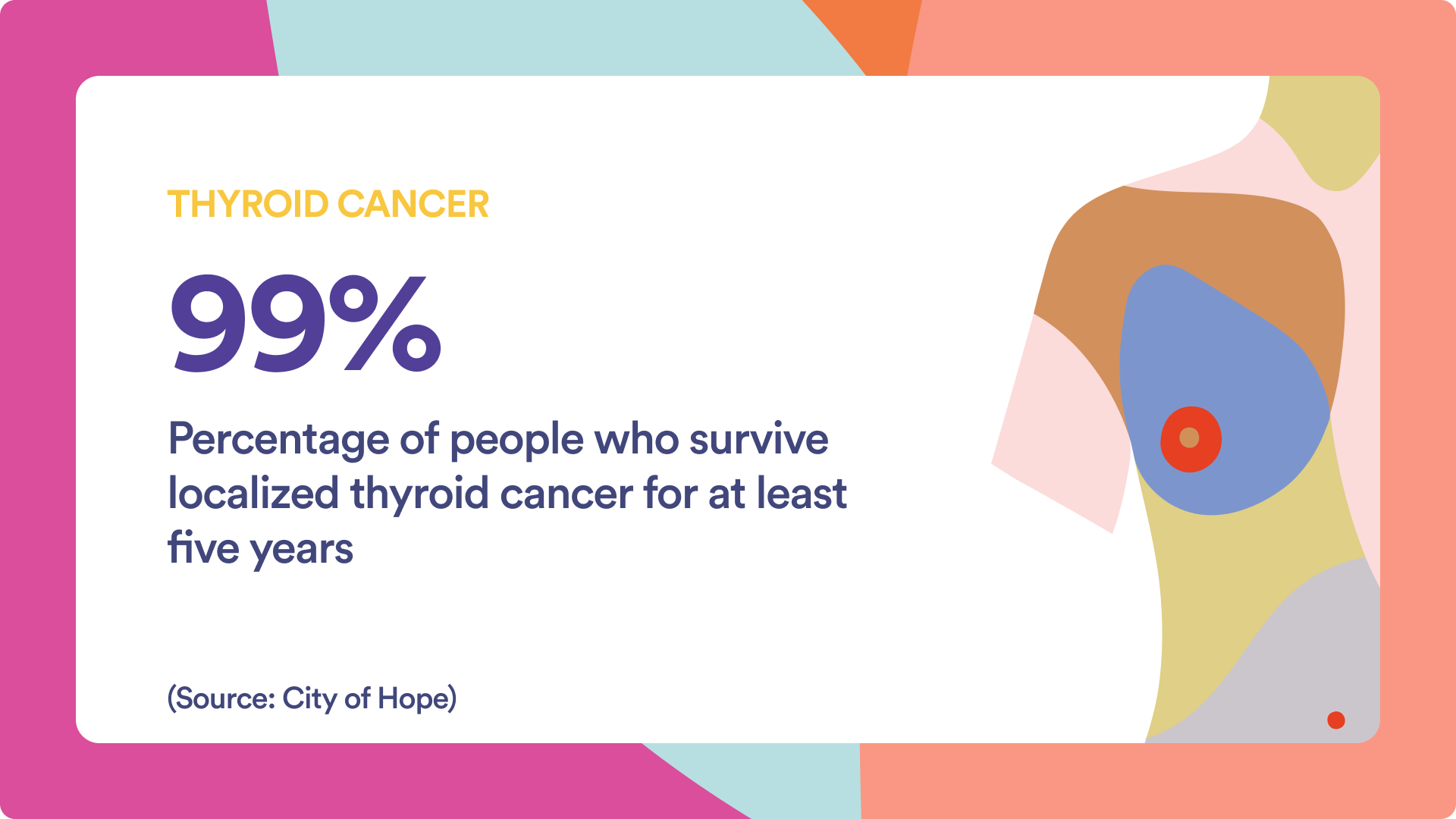
- Papillary Thyroid Cancer (PTC): This is the most common type, making up about 80% of thyroid cancer diagnoses. It tends to grow slowly and is highly treatable, with an excellent cure rate. It usually develops in just one part (lobe) of the thyroid. Even when it spreads to nearby lymph nodes, most patients do very well with treatment. Papillary Thyroid Cancer has a near-100% five-year survival rate if found early and still localized. Even when it spreads, the survival rate is very encouraging.
- Follicular Thyroid Cancer: This is the second most common, making up about 10% of thyroid cancers in the U.S. It can spread through the bloodstream to lungs or bones. It still usually grows slowly and often responds well to treatment. Follicular Thyroid cancers have excellent long-term outcomes when diagnosed early.
- Oncocytic Thyroid Cancer (Hürthle Cell Cancer): This is a less common type once considered part of follicular cancer. It can be more challenging to treat but, if detected early, outcomes can still be good.
“Although papillary thyroid cancer is the most common, the other types of cancers tend to be more aggressive and tend to spread more widely, at least in advanced cases,” Dr. Lisa Orloff, a head and neck surgeon at Stanford Medicine, explains.
Non-differentiated Thyroid Cancers
Non-differentiated cancers can come from follicular cells that are so mutated that they no longer look much like thyroid cells under a microscope.
- Medullary Thyroid Cancer (MTC): This type of cancer arises from the C cells of the thyroid, which make the hormone calcitonin. These make up about 2% to 5% of all thyroid cancers and can sometimes be inherited (through changes in the RET gene). This inherited form, called Multiple Endocrine Neoplasia type 2 (MEN2), can appear in childhood or early adulthood. MTC can spread to lymph nodes, lungs, or liver before a noticeable thyroid nodule appears. The prognosis for MTC depends on how early it’s found and whether it’s inherited or sporadic. Ongoing research and targeted therapies show positive results for many.
- Anaplastic Thyroid Cancer: This is the rarest and most aggressive type, making up about 1% to 2% of all thyroid cancers. It occurs mostly in older adults and often grows and spreads rapidly, sometimes from a pre-existing papillary or follicular cancer that has gained new mutations. It can be hard to treat successfully, but a combination of surgery (if possible), chemotherapy, targeted therapy, and radiation may help slow progression.
“Medullary thyroid cancer is a completely different cell of origin,” Dr. Orloff explains. “Medullary cancer is treated with surgery. There are targeting agents that can treat it when it’s wide-spread. It is monitored through a separate blood test called calcitonin.”
Targeted therapies have also been successful at shrinking aggressive anaplastic thyroid cancers, Dr. Orloff explains, to the point where they can be surgically removed.
“Then the patient can go onto have additional chemotherapy and radiation therapy and can actually achieve a cure,” she says. “Anaplastic is a horribly aggressive cancer, but if it’s caught early and it is treated in a multidisciplinary way, it actually has become a type of cancer that can be cured.”
Symptoms & Diagnosis
Early Signs and First Appointment
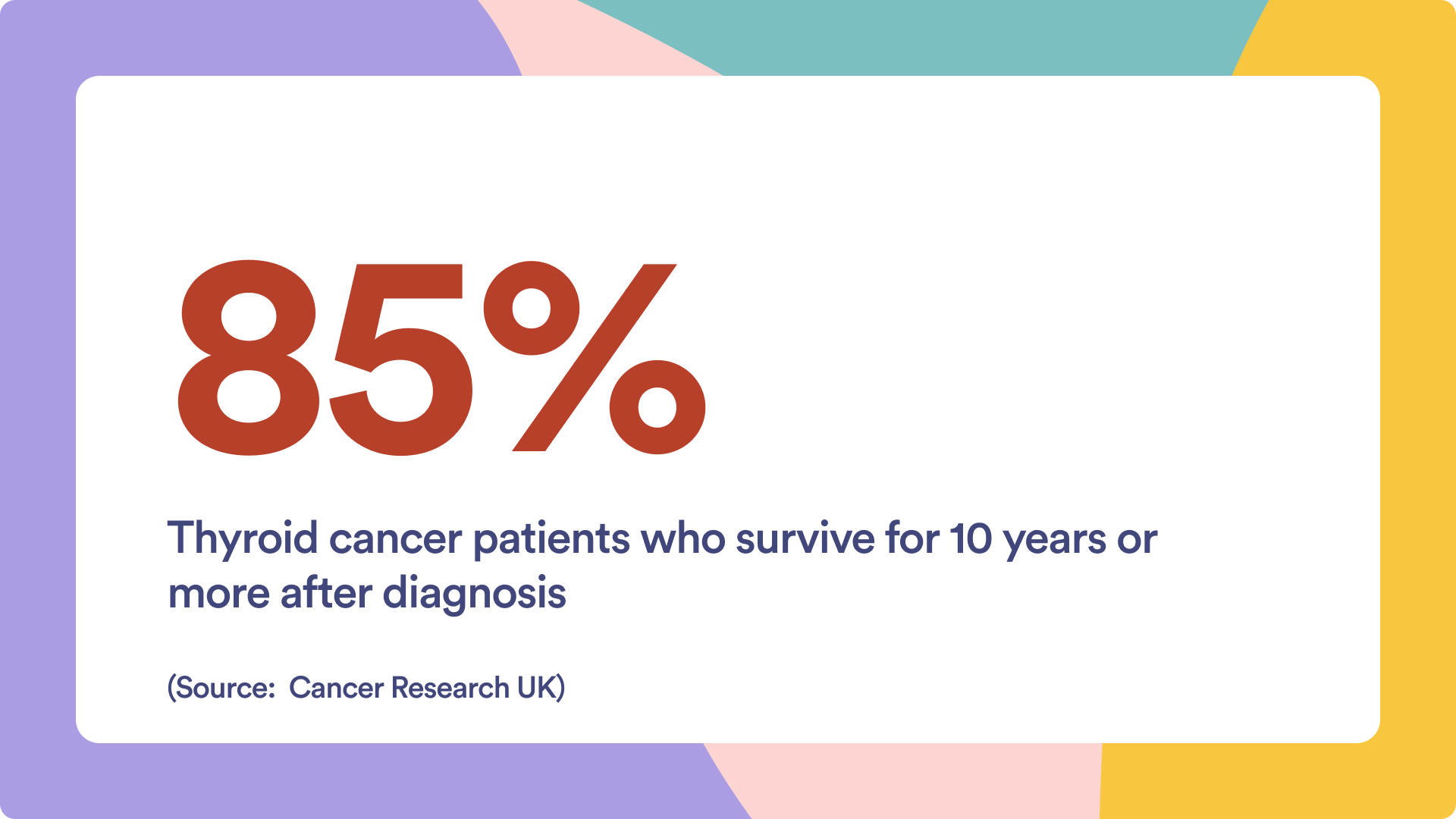
While facing a thyroid cancer diagnosis should not be belittled, keep in mind that thousands of people are diagnosed with thyroid cancer each year in the United States, and most will go on to successfully complete treatment and return to normal lives.
Your first appointment with a physician is a vital step in sorting out whether changes in your neck area or other suspicious symptoms, like changes to your voice or difficulty swallowing, point to thyroid cancer or a less serious condition.
“The development of lumps in the thyroid or nodules is very common,” says Dr. Orloff
“The majority of nodules are benign. About 7 to 10% of thyroid nodules, however, are cancerous. And part of the challenge is identifying which nodules are cancerous compared to the majority.”
“Thyroid nodules are something that we all deal with increasingly over our lifetimes. So there’s sort of a general statistic that by the age of 50, about 50% of adults will have some thyroid nodularity, and some of that nodularity is not detectable to the individual. It’s found on imaging studies, for example,” she adds.
It is worth noting that thyroid cancer can be diagnosed at an age younger than most people are even thinking about the possibility of a cancer diagnosis, even in childhood. To detect cancer early and have a better chance of successful treatment, it’s important to be aware of signs and symptoms.
+ Expand and Learn More About Possible Symptoms ...
Early Signs of Thyroid Cancer
“Sometimes there could be no sign at all,” Giparas tells SurvivorNet.
“Sometimes the patient could go in for imaging, especially at a cancer center for just surveillance follow-up, and they could find an incidentally noted thyroid nodule. Other times when patients usually present with symptoms, usually it’s a lump on either the thyroid gland or enlarged neck lymph node.”
Here’s a breakdown of possible symptoms to be aware of:
Neck Lump or Nodule
One of the most common early signs of thyroid cancer is a lump or nodule in the neck area. You might spot this lump yourself when looking in the mirror or notice it when swallowing. Sometimes, doctors will detect it during a physical exam or imaging test done for another reason.
Thyroid nodules are typically painless. If a nodule is small, you might not notice it at all. Some nodules can grow large enough that they become visible or you can feel them with your fingertips.
Sometimes, thyroid cancer may cause lymph nodes in your neck to swell. Lymph nodes often enlarge for a variety of reasons, including infections. However, if they stay enlarged for a prolonged period without improvement, you should consult a healthcare provider.
Most nodules are actually benign (non-cancerous). Only a small percentage turn out to be thyroid cancer.
Changes in the Voice (Hoarseness)
“If somebody does have symptoms related to a thyroid cancer, that’s usually an indication that it’s a more advanced cancer,” Dr. Orloff explains.
The thyroid gland is close to your voice box (larynx). A growing thyroid nodule, particularly one pressing on the nerves controlling your vocal cords, may lead to hoarseness, persistent voice changes, or difficulty projecting your voice.
Many non-cancerous conditions, such as colds or laryngitis, can cause hoarseness as well. But if your voice remains hoarse longer than a few weeks without clear reason, a medical evaluation is a good idea.
Trouble Swallowing or Breathing
As a thyroid mass enlarges, it can press on your esophagus (the tube that carries food to your stomach) or your windpipe. This pressure might make it feel harder to swallow or breathe.
Difficulty swallowing doesn’t always mean you have thyroid cancer. Still, breathing or swallowing changes should not be ignored.
Diagnosis
Once you suspect something — maybe a small lump in your neck, or persistent hoarseness — it’s time to see a healthcare provider. Many people start with either a primary care physician (such as a family doctor) or go directly to an endocrinologist, who specialize in hormone-related glands (including the thyroid). You might also see an otolaryngologist (an ENT doctor) if your main complaints involve voice changes, swallowing problems, or lumps in the neck.
“When anyone comes in and they hear the word cancer, our brain just elicits a panic mode. What does this mean for me and the long-term aspects of my life or my health?” Giparas says.
“It’s really important to talk about what the normal pathophysiology or how thyroid cancer behaves and it’s risk to them in their lifetime. If this is caught quite early, and if it’s a small tumor, a lot of patients can just undergo the surgery and they can live their whole life without any issues, except potentially surveillance to make sure that it’s completely treated.”
Your doctor will perform a series of tests to determine if you have thyroid cancer, what type, and how aggressive it is. This will help determine the best treatment path for you.
+ Expand and Learn More About Thyroid Cancer Diagnosis ...
Before your appointment, it’s generally a good idea to prepare in the following ways:
- Gather Records: If you have had any relevant tests — like neck ultrasounds or blood tests — bring those results with you.
- Write Down Symptoms: Note anything unusual, no matter how minor. This includes changes in energy, mood, weight, appetite, voice, or swallowing.
- Family History: If possible, find out if any close relatives have had thyroid cancer or other endocrine-related conditions. This background can be crucial.
This initial appointment can be nerve-racking, but remember: your doctor or specialist is there to help you.
Here are some steps typically involved in the first meeting:
- Discussion and Questions: You will have time to describe your symptoms, concerns, family history, and any relevant lifestyle factors. Don’t be shy — this is the moment for honesty and detail.
- Physical Exam: Your doctor may gently feel your neck for nodules or enlarged thyroid tissue. They might also check your lymph nodes and look for signs of difficulty swallowing or breathing.
- Blood Tests: Common tests measure levels of T3, T4, and TSH. These results will indicate if your thyroid is overactive, underactive, or functioning normally. If medullary thyroid cancer is suspected, your doctor might also check levels of calcitonin and a substance called carcinoembryonic antigen (CEA).
- Imaging: Often, an ultrasound of your thyroid and neck area will be scheduled. Ultrasound is non-invasive and can show whether nodules are solid or filled with fluid, as well as check nearby lymph nodes. In some cases, a scan using radioactive iodine helps determine if the nodules are “hot” (producing excess hormone) or “cold” (less active, with a higher chance of being cancerous).
“Ultrasound is the best method for evaluating characteristics of thyroid nodules, and there are features that are suggestive of malignant changes, and there are other features that are more reassuring and suggestive of benign changes,” Dr. Orloff explains.
“However, no ultrasound can absolutely confirm or rule out a cancer. And even if suspicious changes are present, there are different cancer subtypes. So the needle biopsy is the step that follows the diagnostic ultrasound.”
Fine-Needle Aspiration (FNA) Biopsy
Your doctor may also recommend a fine-needle aspiration (FNA) biopsy.
“The needle biopsy retrieve cells from a nodule, and those cells are first examined by a pathologist for their architecture or their structure. And so most diagnoses of thyroid cancer can be made through what’s called cytopathology or looking at the cell structure and the individual nuclei within cells,” Dr. Orloff explains.
Here’s a breakdown of the FNA process:
- Preparation: You’ll be asked to lie down or sit in a comfortable position. If the FNA is for your thyroid, you’ll typically lie on your back with your neck slightly extended. This position makes the area easier for the doctor to see and reach. The skin over the area is cleansed, and sometimes a local anesthetic is applied so you won’t feel as much discomfort.
- Guidance by Ultrasound: “Needle biopsies are usually done under ultrasound guidance, and so the same tool ultrasound that is used to characterize nodules is used to help target a nodule for biopsy,” Dr. Orloff explains. Ultrasound is a safe imaging method that uses sound waves (no radiation). By using ultrasound, the doctor can clearly see the lump’s exact size and location. This helps ensure that the needle goes into the correct spot and collects the right cells.
- Inserting the Needle: A thin, hollow needle — much smaller than the one used for drawing blood — is gently inserted into the lump or nodule. The doctor will move the needle in a slight back-and-forth motion to gather cells. It may feel like a small pinch or mild pressure. Most people tolerate this very well and say it’s only minimally uncomfortable.
- Collecting the Cells: The needle is attached to a small syringe, and your doctor or technician may or may not need to apply gentle suction to pull cells into the syringe. The needle is usually in place for only a few seconds.
- Releasing the Sample: Once enough cells or fluid have been collected, the needle is carefully removed. The sample is placed on a slide or in a container and sent to a pathology lab, where a specialist (pathologist) examines the cells under a microscope.
- After the Procedure: A small bandage may be placed over the spot where the needle went in. Most people can go back to their usual activities almost immediately. Mild soreness at the site is possible but usually goes away quickly. If the area feels tender, an over-the-counter pain reliever might help.
Surgery
Surgery: Thyroid Removal
Surgery is the cornerstone of the treatment path for people facing thyroid cancer — and it’s natural to have questions and feel anxious about the surgery process.
Types of Thyroidectomy
“Historically most thyroid cancers were treated with complete thyroid removal, so total thyroidectomy and then follow up care with radioactive iodine,” Dr. Kristen Otto, head and neck surgeon at Moffitt Cancer Center in Tampa, Florida, tells SurvivorNet.
“We now understand and have moved much more on the opposite end of the spectrum, away from these more aggressive procedures to trying to do more limited procedures like partial thyroidectomy.”
How much of your thyroid is removed depends on the reason for the surgery, the size of the affected area, and the type of thyroid disease present.
Total (or Near-Total) Thyroidectomy
- What Is It? In this procedure, the entire thyroid gland is removed. In a near-total thyroidectomy, only a tiny part of thyroid tissue is left behind, but this is less common.
- Who Needs It? People with more advanced thyroid cancers, those who have large goiters, or people who have multiple areas of concern in their thyroid might need this.
- After-Effects: Since the entire gland is gone, your body will no longer produce its own thyroid hormone. You will need to take synthetic thyroid hormone pills (most commonly levothyroxine) every day to replace the hormones your thyroid once made.
Partial Thyroidectomy
- What Is It? In this procedure, only a portion of the thyroid gland is removed. This could be a hemithyroidectomy (thyroid lobectomy), where the surgeon removes one lobe (half) of the gland, or a isthmusectomy, where only the thin piece of tissue (isthmus) that connects the two lobes is removed. This is less common, typically considered if a small tumor sits in that narrow band.
- Who Needs It? People who have a nodule confined to one side or who have smaller growths that only affect a portion of the thyroid may be candidates.
“The benefits to partial thyroidectomy over total thyroidectomy are that many patients maintain normal thyroid function and don’t have to be on lifelong thyroid hormone medication after a partial thyroidectomy, whereas with a total thyroidectomy, you need the lifelong medication,” Dr. Otto explains.

+ Expand and Learn More ...
“Additionally, it’s shorter surgery and less invasive, so we do prefer partial thyroidectomy. There are some patients who are well suited to that, and then there are others who are not, and we can go over those details,” Dr. Otto adds.
She notes that tumors that are small and on one side of the gland are well-suited for a partial thyroidectomy.
“We really need a small tumor that is isolated to one lobe and doesn’t cross over the midline in order to be appropriate for that procedure. Most guidelines, NCCN and the American Thyroid Association suggests that patients with tumors under four centimeters are appropriate candidates for partial thyroidectomy,” she adds.
Thyroidectomy is generally considered safe, especially when performed by a skilled and experienced surgical team. Even so, every operation carries some risk.
“The surgery itself is complex and delicate, but yet, it’s also a surgery that most people recover from very quickly,” says Dr. Lisa Orloff.
+ Expand and Learn More On The Risks of Thyroid Cancer Surgery ...
The most common complications associated with surgery include:
- Nerve issues impacting the voice and swallowing
- Voice hoarseness or weakness due to nerve issues
- Hypoparathyroidism (Low Parathyroid Hormone)
- Bleeding
- Infection
- Esophageal or Tracheal Injury
- Difficulty Swallowing (Dysphagia)
Nerve Injury
“The thyroid gland is very intimately associated with the nerves that control vocal cord movement. So in any thyroid operation, there’s a possibility of injury, either temporary or permanent, more often temporary,” Dr. Orloff explains.
If the vocal cord nerves — the laryngeal nerve, the recurrent laryngeal nerve or the smaller superior laryngeal nerve — is affected, there can be a change in voice quality and control of vocal cord muscle, which Dr. Orloff notes can affect swallowing, coughing, projection, and even breathing.
“It’s important to have a dialogue between the patient and the surgeon and acknowledge the importance of those nerves and the aim to protect those nerves as much as possible. The rate of injury is very, very low, but it is something that needs to be prioritized,” she explains.
During intraoperative nerve monitoring, if the monitor picks up a concern on the first side, your surgeon may complete that one side and then stop the surgery to give that nerve time to heal before taking on the second side.
Recurrent Laryngeal Nerve Injury
- Why It Matters: the recurrent laryngeal nerve controls your vocal cords. If it’s harmed, you could experience changes in your voice or, in very rare circumstances, breathing difficulties if both nerves are affected.
- Causes: This nerve can be bruised or accidentally cut, especially if the cancer or enlarged gland is wrapped around it. Even gentle stretching can temporarily affect nerve function.
- Signs and Symptoms
- Hoarseness: Your voice might sound weak, breathy, or harsh due to nerve issues.
- Trouble Swallowing: As the recurrent nerve is also responsible for some of the sensory functions in our throat, we may not always feel the normal triggers to start the swallowing events.
- Weakened Cough: You might not be able to clear your throat as strongly
- Aspiration: The vocal cords may not close completely to protect the airway when you swallow. Thin liquids like water can sometimes drip down to irritate the vocal cords or even slip past them.
- Prevention and Management: Many surgeons use special devices, intraoperative neuromonitoring, to help them pinpoint the nerve’s location, lowering the chance of harm.
- Recovery: Most nerve injuries are temporary, lasting weeks to months. If the nerve is severely damaged, voice therapy or an additional procedure might be needed.
- Voice Rehabilitation: A specialist such as a speech-language pathologist can help you strengthen your voice if you experience ongoing issues.
Superior Laryngeal Nerve Injury: Less Obvious but Significant
The external branch of the superior laryngeal nerve plays a role in voice pitch and singing. When injured, it might be less noticeable than recurrent laryngeal nerve damage, but it can still affect your ability to raise your voice or sing high notes.
Studies show varying rates of injury because patients may not realize they have an issue, especially if they don’t regularly use a wide vocal range.
If you notice changes in your ability to speak or sing at higher pitches, mention them to your doctor. Sometimes voice therapy helps, but injuries may be long-lasting.
Low Calcium
“The other structure that may not have been even something people have heard of but is present next to the thyroid gland are these little tiny glands called parathyroid glands. Parathyroid glands produce a separate hormone called parathyroid hormone that regulates calcium levels in the blood. And this is another function of the body that when it’s working fine, we aren’t even aware of it. But if we have a low level of calcium in our blood, we can develop muscle cramps and numbness and tingling and even more changes in muscles like the heart,” Dr. Orloff explains.
Low parathyroid hormone levels can cause low calcium levels in the blood. If the parathyroid glands are damaged during surgery, a patient may need to take calcium supplements. These supplements may be taken alongside vitamin D supplements, Dr. Orloff says. These supplements are typically temporary.
“Calcium and vitamin D are usually temporary. The parathyroid glands, there are typically four of them, and they aren’t all necessarily affected by a thyroid surgery. So as long as somebody has a functioning parathyroid gland, they usually recover control of their calcium balance spontaneously,” she adds.
When calcium levels in the blood fall too low, you might notice:
- Tingling or numbness in the fingers, toes, and around your lips
- Muscle cramps or spasms
- In severe cases, difficulty breathing or painful muscle contractions called “tetany”
Your care team will measure your calcium levels frequently in the hours or days after surgery. Many hospitals use a “calcium protocol” to catch drops quickly.
Surgical teams may measure the parathyroid hormone level after surgery as a predictor of who will need calcium supplementation and monitoring.
Most people recover normal parathyroid function within a few weeks if the gland was only “stunned” or bruised. But if the glands were significantly damaged, you may need lifelong calcium and vitamin D to avoid symptoms.
Hemorrhage (Bleeding)
Postoperative bleeding isn’t very common, but it’s among the more serious risks.
- Why It Occurs: The thyroid gland has a rich blood supply. If a blood vessel reopens or wasn’t fully sealed during surgery, blood can collect rapidly in the neck area.
- Potential Danger: A large, rapidly forming hematoma (a collection of blood outside the blood vessels) can press on your windpipe, making it difficult to breathe.
- Symptoms: Sudden neck swelling, difficulty breathing, and/or a feeling of tightness or choking in the throat area.
- Immediate Action: Nurses and doctors will often check your incision frequently during the first hours after surgery, partly to look for signs of bleeding. If severe bleeding occurs, the surgical incision may be reopened to relieve pressure and stop the bleeding. In a dire emergency, this might happen right at the bedside rather than in an operating room.
- Outlook: Though hemorrhage can be frightening, quick intervention often resolves the problem. You may need another brief operation to ensure there are no more leaks.
Infection
Typically under 1% of thyroidectomy patients can develop an infection at the incision site. The frequency is generally low, but this can vary depending on your overall health, the specifics of the procedure, and hospital practices. It is more likely to see skin reactions due to surgical dressing or the surgical prep than true infections.
Signs of infection might include:
- Redness
- Warmth
- Swelling at the incision
- Fever
- Pus (if the infection is serious)
It is typically treated with antibiotics. Good surgical technique and proper wound care lower the risk.
Esophageal or Tracheal Injury
Though rare, accidental injury to these structures can happen if the thyroid growth is stuck to or pressing on them.
If recognized quickly, surgeons can repair the injury. Delayed recognition can lead to complications like infection in the chest, so careful postoperative monitoring is important.
Difficulty Swallowing
Dysphagia is a temporary swallowing issues that can result from normal swelling and scarring.
Most people improve gradually. Persistent swallowing problems may need further evaluation or speech therapy.
Although these complications can be alarming to read about, it’s important to remember that they are either rare or usually manageable. Experienced surgeons and careful postoperative monitoring help catch problems early so they can be treated promptly.
Common Treatment
What is Radioactive Iodine (RAI) Therapy?
After surgery, which is the most common treatment, many patients with advanced disease benefit from Radioactive Iodine (RAI) Therapy. In our extensive interviews with thyroid specialists at leading cancer centers, we found this targeted approach is frequently recommended.
As an endocrine organ, the thyroid gland plays a crucial role in orchestrating our metabolism. Producing thyroid hormones is fundamental to maintaining the overall function and harmony within our body.
Radioiodine therapy aims to kill off overactive, residual normal or cancer cells to treat thyroid cancer and hyperthyroidism, which occurs when your thyroid gland makes too many hormones. The treatment aims to kill off overactive thyroid cells.
The treatment dose depends on how much cancer your medical team believes is left over.
+ Expand and Learn More ...
“The first thing we do is we have patients go on a low iodine diet for a couple weeks before the treatment, usually two weeks before the treatment, and typically our nurses will educate patients on what foods they have to avoid to make sure that their body iodine stores are extremely, extremely low,” Dr. Otto explains.
“The treatment is a kind of process that lasts about three or four days, essentially. [For] the first two days, patients get the thyrogen injections [a protein designed to be identical to the natural thyroid-stimulating hormone, or TSH, our bodies make], and then on the third day, most patients will be given a small dose of radioactive iodine and they’ll have a head to toe scan, and we look for any uptake and that allows us to prepare the treatment dose.”
“If we see some uptake in just in the neck alone, which we almost always do, even after the best thyroid surgery, we’ll see just a little bit of uptake in the neck, then we know we can treat with a slightly lower dose,” Dr. Otto explains. “If we see uptake outside the neck, for instance, in the lungs, then we assume that the thyroid cancer has already metastasized to the lungs. And for those patients, we give a higher treatment dose.”
+ Expand and Learn More About Thyroid Hormones ...
Understanding TSH
Thyroid-stimulating hormone, or TSH, generates commands specifically to the thyroid cells to capture iodine in the blood stream and make up thyroid hormones (T3 and T4). Therefore, the presence of TSH makes the thyroid cells capable of performing this work. Technically, the more TSH, the more iodine captured and the more thyroid hormone produced.
Thus, scientists realized that a modified iodine molecule could trick the thyroid cell and promote its death instead of thyroid hormone. When both TSH and iodine are given to a patient, this effect could be enhanced since the presence of TSH would stimulate even more the thyroid cells to absorb this modified iodine (radioactive iodine).
There are two main methods to increase TSH in a patient to stimulate this process: thyroid hormone withdrawal (which will alert the pituitary to release more TSH) or administration of recombinant human TSH.
“We often give patients thyroid hormone supplements, especially if they’ve had their thyroid removed completely, since they need thyroid hormone for normal health. We use recombinant TSH in order to avoid taking away their thyroid hormone and making them hypothyroid [which means they have a low level of thyroid hormones],” Dr. Orloff tells SurvivorNet.
“There has been the development of this recombinant TSH, which is basically a way of injecting a dose or two doses of TSH to artificially or temporarily raise the level of TSH in the blood just long enough to give the person radioactive iodine and … that TSH helps the iodine get into the cells. So, it’s a much more comfortable way in many instances to achieve the treatment with radioactive iodine without having to be deprived of your thyroid hormone.”
Thyroid Hormone Withdrawal
After having your thyroid removed (thyroidectomy) or stopping your usual thyroid hormone medication (like levothyroxine), you allow your body’s TSH level to rise naturally.
This approach requires stopping levothyroxine (T4) for about three to four weeks. However, to make the process easier, one method is to reduce your T4 dose by 50% for four weeks, then stop it completely for one more week. Another method is to switch from levothyroxine (T4) to a shorter-acting form (liothyronine or T3) for a certain period to reduce the time you’re off medication entirely.
“In the past, when we did radioactive iodine therapy, we took patients off thyroid hormone for about six weeks and allowed them to become profoundly hypothyroid. And in most cases, that’s a very miserable feeling… patients are extremely fatigued. They often feel terrible. And so these days we don’t have to do that because we can give this injection of TSH recombinant TSH or thyroid,” Dr. Otto explains.
Possible side effects of hypothyroid (low thyroid hormone) include:
- Fatigue, low energy, and muscle aches
- Feeling colder than usual
- Weight gain or fluid retention
- Mood changes (depression, irritability)
- Slowed thinking or forgetfulness
Recombinant Human TSH (rhTSH)
Now, instead of stopping your thyroid hormone medication, doctors can inject you with a man-made form of TSH (called rhTSH). This makes the thyroid cells (or thyroid cancer cells) “hungry” for iodine, without you going through a low-thyroid (hypothyroid) phase.
You stay on your usual dose of levothyroxine (T4) so you don’t develop low-thyroid symptoms. You get two injections of rhTSH on two consecutive days, and on the third day, you receive the radioiodine treatment. This quickly raises TSH levels, allowing the radioiodine to be effective without long periods of deprived medication.
This approach avoids hypothyroid symptoms because you stay on your usual thyroid hormone, you don’t go through the typical low-thyroid side effects (fatigue, weight gain, depression, etc.).
Although very uncommon, rhTSH can also stimulate the rapid growth of any remaining thyroid cancer cells. This is extremely rare.
New Treatments and Precision Medicine
The Latest Treatment Developments
Precision medicine is an approach that tailors cancer treatments to each individual’s unique genetic profile, rather than relying on a one-size-fits-all plan.
By identifying specific gene changes driving a tumor’s growth, doctors can select therapies that are more likely to be effective and cause fewer side effects.
“The vast majority, over half of all thyroid cancer in the advanced state, harbors some sort of molecular aberration, like a mutation or a fusion protein, that lends itself to different targeted therapies,” Dr. Jessica Geiger, a medical oncologist who specializes in head and neck cancers at Cleveland Clinic, tells SurvivorNet.
This personalized strategy is especially important in advanced thyroid cancer, where finding a precise “target” can mean better outcomes and a greater sense of hope for patients and families.
For some people, these medications are extending life in remarkable ways.
+ Expand and Learn More...
Tailoring Your Treatment Plan
1. Targeted Therapies
When doctors identify a mutation — like BRAF or RET — in your thyroid tumor, they might recommend a targeted therapy designed to block that specific genetic signal. These treatments can often be easier for your body to handle compared to some traditional chemotherapies, though they do have side effects that your medical team will monitor.
Dr. Geiger points to the BRAF mutation as one of the most common markers in advanced thyroid cancer.
2. Immunotherapies
Sometimes, thyroid cancers have genetic or molecular features (like MSI-high or PD-L1 expression) suggesting that they may respond to immunotherapy — drugs that help your immune system recognize and fight the cancer more effectively. While not every thyroid tumor qualifies for immunotherapy, testing helps doctors check whether you’re a candidate.
Clinical Trials
When to Consider Clinical Trials
Taking part in a clinical trial may allow thyroid cancer patients to access the most recent and cutting-edge treatments years before they’re available, and these treatments can include immunotherapy, targeted therapy, gene therapy, or even a new combination of currently used treatments like surgery, chemotherapy, or radiation therapy.
“There is an incredible bevy of new therapies being developed. If I were a cancer patient with a widely spread metastatic cancer, I would want to be on a clinical trial,” Dr. Benjamin Neel, director of NYU Langone’s Perlmutter Cancer Center, explained to SurvivorNet.
Although some drugs tested in trials will fail, they increase the odds for a successful outcome as patients enrolled in clinical trials tend to be monitored more closely.
+ Expand and Learn More...
“The National Comprehensive Cancer Network believes that the best management for any patient with cancer is in a clinical trial,” Dr. Mariam Eskander, a surgical oncologist and Assistant Professor of Surgery at the Rutgers Cancer Institute of New Jersey, told SurvivorNet.
“Clinical trials are not the last resort — they can actually be a first resort,” she added. “And so I bring them up early. I include them in the list of treatment options I have for a patient.”
Although there’s no guarantee that newly offered treatments will produce great results in curing thyroid cancer, at the very least, it can ensure proper care and follow-up from the healthcare team running the trial.
There’s also the knowledge that you’ll be helping doctors make ground-breaking discoveries and produce much-needed treatments empowering other patients like you.
Additionally, many of the fees or added costs that are directly related to the trial will be covered by insurance or the trial, so you will often not have to pay to get treated.
Follow-Up Care and Surveillance
Thyroid Cancer Surveillance — How Will I Be Monitored After Treatment?
After completing treatment for thyroid cancer (which may involve a combination of surgery, radioactive iodine therapy, or other treatments), you will be carefully monitored by your treatment team — medical professionals call this “surveillance.”
This period of close monitoring is crucial to detect any potential recurrence of thyroid cancer early when it’s most treatable. It also allows you to ensure thyroid hormone levels remain in the proper range (especially if you’re on hormone replacement), assess overall health, and address any side effects from the treatment.
Frequency of Follow-Up Care
Generally speaking, we can frame the frequency of follow-up in two main periods: the first year following treatment and beyond the first year. However, this is not a one size fits all rule, and patients may need more or fewer appointments according to their progress and needs.
“Anybody who has a diagnosis of thyroid cancer, who’s been treated for thyroid cancer, we do less frequent surveillance for low risk disease, a little bit more frequent for intermediate risk and much more frequent for high risk,” Dr. Otto tells SurvivorNet.
+ Expand and Learn More on Monitoring ...
First Year After Treatment
In the first year after completing treatment, it’s common to see your doctor every three to six months. Most patients see their doctor (often an endocrinologist or oncologist) more frequently at the beginning.
These visits allow for close monitoring of hormone levels, ensuring you’re on the correct dose of thyroid hormone replacement and quickly addressing any unusual symptoms.
Beyond the First Year
- If All Results Are Stable: Your doctor might gradually reduce the frequency to every 6-12 months.
- Longer-Term Survivorship Care: If there’s no sign of recurrent cancer over a period — often several years — your doctor may decide to extend the interval to annual visits or possibly transition your care to a primary care physician, with occasional check-ins with a specialist.
The exact timing can vary widely. More aggressive or advanced cancers may require longer and closer surveillance, while small, low-risk cancers may allow for less frequent appointments once you are in remission.
“We know that for papillary thyroid cancer, if someone is going to have a recurrence, most likely it’s going to happen within the first five years. [The] highest percentage happen within the first three years, but we know out to five years we’ll catch 97 to 99% of recurrences,” Dr. Otto explains.
+ Expand and Learn More...
Common Tests and Evaluations
At your follow-up visits after treatment, your doctor will perform a series of tests to assess your overall health.
“The surveillance includes blood work, ultrasound, and office visit. Sometimes for the high risk patients, we add in scans because we can’t see, for instance, lung metastases on an ultrasound of the neck, we’d have to get a scan of the chest,” Dr. Otto explains.
Your healthcare provider will likely use a combination of the following tools and tests:
Blood Tests
- TSH (Thyroid-Stimulating Hormone): Helps your doctor see if your thyroid hormone replacement dose needs adjusting
- Free T4 (FT4): Another measure of thyroid hormone in your blood
- Thyroglobulin (Tg): After thyroid removal (and sometimes radioactive iodine), levels of thyroglobulin (a protein produced by thyroid cells) should be very low or undetectable. Rising levels may signal potential recurrence.
Neck Ultrasound
Ultrasound imaging of the neck is used to check for any suspicious lumps or lymph nodes. This is a key test in detecting local recurrences.
Imaging Tests (If Needed)
Sometimes other imaging (such as CT, MRI, or a radioactive iodine scan) may be recommended, especially if there are elevated thyroglobulin levels without a clear source.
Transitioning from Specialist to Primary Care
Many patients wonder when, if ever, they can leave the care of their oncologist or endocrinologist and return to primary care follow-up (seeing their local doctor).
This decision is highly individualized but typically involves:
- Consistency in “No Evidence of Disease”: If you’ve gone several years with stable, low (or undetectable) thyroglobulin levels, normal imaging results, and no suspicious symptoms, your doctor may consider reducing the frequency of specialist visits.
- Low-Risk Cancer: Individuals with smaller, low-risk thyroid cancers often have a smoother transition back to primary care, provided they remain stable.
- Shared Care Model: Sometimes, you may continue to see a primary care provider for routine health needs and an endocrinologist or oncologist once a year (or less) to monitor hormone levels and check for any signs of recurrence.
“If we follow a patient out through five years and there’s no evidence of disease at that point, at Moffitt Cancer Center, we generally then graduate our patients to back to their primary care doctor or to our survivorship program where they’re getting more long-term [care],” Dr. Otto says.
Your medical team will guide you on the safest timeline. They’ll make sure you understand the signs or symptoms that should prompt you to return to specialist care more quickly.
Knowing What to Watch For
Patients should monitor their health for any changes that may warrant a visit to the doctor, even when they are on a regular monitoring schedule.
Experts recommend the following:
- Keep an Eye on Any Neck Changes: Report new lumps, swelling, or discomfort in the neck to your doctor.
- Stay Alert to Thyroid Hormone Imbalance Symptoms: Fatigue, weight changes, temperature intolerance, or unusual heartbeat patterns can indicate a dosage issue with your thyroid medication.
- Stay in Contact with Healthcare Providers: Don’t wait for your next scheduled appointment if you have concerns. Reach out sooner.
Recurrence
What Are My Options If Cancer Returns?
Even though the prospect of a recurring (returning) cancer is frightening, it’s important to know that there are effective treatments available. Many people go on to manage, or even eradicate, recurrent thyroid cancer successfully, living long, fulfilling lives.
“Recurrence usually is detected in one of two ways. Either they have a new finding on imaging, so we’re likely doing surveillance ultrasounds of their neck or CT scans and something pops up that wasn’t there before. Alternatively, sometimes we detect a recurrence through the blood work,” Dr. Samantha Kass Newman, an endocrinologist at Memorial Sloan Kettering Cancer Center, tells SurvivorNet.
After initial treatment, thyroid cancer patients are carefully monitored for recurrence — and if the cancer does come back, there are still treatment options available. Survival rates are still very good for most people, and new treatments continue to provide hope for long-term remission.
Why Thyroid Cancer Sometimes Comes Back
Even with high treatment success rates, thyroid cancer can recur. Depending on the source, about 20% of people with thyroid cancer are at risk of having it come back after initial treatment. Recurrence may happen a few months after remission or it could surface years — sometimes even decades — later.
+ Expand and Learn More About Recurrence Risks ...
Certain factors that may increase the risk of thyroid cancer returning include:
- Age over 55 at the time of initial diagnosis
- More aggressive or advanced stage tumor (for example, a tumor that has spread beyond the thyroid or has invaded blood vessels)
- Being male (though women are more likely to get thyroid cancer in general, men who do get it sometimes face a higher risk of recurrence)
- Specific genetic changes, such as mutations in the BRAFV600E gene
- Incomplete surgical removal of the original cancer if the tumor was too large or in a location that was difficult to remove entirely
Although these factors can increase one’s chances of facing a recurrence, they do not mean a recurrence is inevitable. Many people in higher risk groups never experience a return of their disease, while some in lower risk groups may find the cancer comes back unexpectedly. The true risk varies by individual.
“When we say low-risk or high-risk cancer, we really mean risk of recurrence,” Dr. Newman explains. “So not risk that it’s going to limit your lifespan or risk that you may die of your disease. It means risk that the cancer is going to come back — and so the low-risk thyroid cancer really means low risk of recurrence.”
Lower-risk patients are usually those whose tumors could be completely removed by surgery and that did not present with any characteristics that might increase the risk that some cancer was left behind, Newman explains.
Type Matters
Thyroid cancer is generally grouped based on the specific cells it develops from and recurrence rates for thyroid cancer also vary according to cancer type.
Papillary thyroid cancer (PTC) has been shown to recur in around 1.6% of low-risk patients, 7.4% of intermediate-risk patients, and 22.7% of high-risk patients, while follicular thyroid cancer recurs in about 13.6% of cases.
Medullary thyroid cancer (MTC) can return in up to 50% of individuals, and Hürthle cell cancer can recur in about 12-33% of cases. Though these figures may appear intimidating, close monitoring and an array of available therapies still provide a favorable outlook for many patients, including those in higher-risk groups.
Treatment Options
There are still several treatment options when thyroid cancer recurs — including additional surgery, radiation therapy, radioactive iodine therapy, chemotherapy, targeted therapy, or even a watch and wait approach.
“We first make a decision about what’s the volume of disease we think we’re dealing with. Sometimes if the volume of disease is very low, even if we suspect a recurrence, we don’t always treat it,” Dr. Newman explains. This is known as a watch and wait approach.
“We really try to not aggressively intervene on very low volume disease knowing what we know about thyroid cancer, which is that we have these periods of very slow growth or no growth that might not warrant aggressive intervention,” she explains.
+ Expand and Learn More About Treatment Options at Recurrence ...
Surgery (Salvage Surgery)
If your recurrent tumor is localized — meaning it’s confined to the neck area and can be safely removed — your doctor may recommend another operation.
Some people undergo compartmental neck dissection if the cancer has returned in lymph nodes in the central or lateral areas of the neck. In other cases, surgeons might remove any suspected residual thyroid tissue or tumor growth that’s close to the site of the initial surgery.
“If someone has a local recurrence in the neck, we always ask our surgeons for their opinion about whether or not this is worthy of another surgery. They’ll go in, they can do a neck dissection, where they clean out the recurrent disease. Sometimes that’s all that’s required,” Dr. Newman explains.
External Beam Radiation Therapy (EBRT)
This treatment may be appropriate in cases where the tumor is inoperable or does not respond to radioactive iodine.
EBRT can help reduce tumor size, alleviate symptoms (like pain or trouble swallowing), and keep the cancer from spreading further.
“Once in a while, we use external beam radiation, which is kind of traditional radiation, where we radiate the field of disease recurrence. We choose those patients really carefully. We don’t like to do things that cause significant side effects, but it is necessary sometimes. Our radiation techniques for external beam radiation become more honed and we’re able to radiate smaller areas and minimize side effects,” Dr. Newman explains.
Radioactive Iodine (RAI) Therapy
For papillary or follicular thyroid cancer, RAI remains a powerful option if the recurring tumor is capable of taking up iodine. If you have small, scattered metastases in the lungs or bones that still absorb iodine, multiple rounds of RAI may help shrink or even eliminate the cancer.
“Radioactive iodine is probably the most targeted form of radiation that exists. It takes into account what we know about the behavior of thyroid cells. Thyroid cells — both healthy and some cancerous — have on their surface a channel called the sodium iodide symporter. This is how the thyroid cell internalizes iodine, which is one of its primary jobs in the body. Thyroid cells need iodine. They use it to make thyroid hormone,” Dr. Newman explains.
“…We can kind of capitalize on this knowledge about how the thyroid cell behaves to get radiation directly into the thyroid cell. Now, one of the most important things that we do when we’re looking at more advanced tumors is look at the mutational status because some mutations that we see in thyroid cancer actually cause a downregulation of those very channels on the cell surface. These are people who are less likely to internalize that iodine and less likely to respond. But assuming someone has a classical papillary thyroid cancer, they may be a candidate for this type of treatment,” she adds.
Chemotherapy
Traditional chemotherapy is not used frequently for thyroid cancer, but in certain advanced cases — particularly those that are aggressive or do not respond to RAI or surgery — it may be offered.
Targeted Therapy
For advanced or RAI-refractory thyroid cancers, targeted medications known as tyrosine kinase inhibitors (TKIs) may be considered. Examples include lenvatinib, sorafenib, cabozantinib, and others.
Targeted therapy is a treatment approach that focuses on the specific genetic changes that drive thyroid cancer cells to grow in unusual ways. Doctors begin by analyzing samples of a patient’s cancer cells, looking for mutations in certain genes, like RET, BRAF, or NTRK.
“The vast majority, over half of all thyroid cancers in the advanced state, harbor some sort of molecular aberration like a mutation or a fusion protein that lends itself to different targeted therapies,” Dr. Jessica Geiger, a medical oncologist at Cleveland Clinic Cancer Center, tells SurvivorNet. “The most common, I would say in advanced thyroid cancer, is BRAF mutation.”
These detailed tests help specialists in pathology and personalized diagnostics pinpoint the exact abnormal signals in each patient’s cancer. Once these changes are identified, a team creates a targeted treatment plan tailored to each individual. The aim is to block the precise proteins or pathways that are causing thyroid cancer cells to thrive, while limiting harm to healthy cells.
Several classes of targeted drugs are available, each designed to shut down different cancer-driving mechanisms.
- Kinase inhibitors (including multikinase inhibitors) work by halting the signals that tell cancer cells to grow or form new blood vessels.
- BRAF inhibitors, often paired with MEK inhibitors, target changes in the BRAF gene, preventing a protein from sending growth signals throughout the cell.
- NTRK inhibitors counteract genetic alterations that affect nerve-related proteins. Similarly, RET inhibitors address mutations in the RET gene, shutting down abnormal proteins in thyroid cells. By customizing which drug — or combination of drugs — is used, doctors can more effectively slow or stop thyroid cancer progression and improve outcomes for many patients.
Some of these medications have side effects that need close monitoring, but they have significantly improved options for those who might otherwise have few treatments.
Thermal Ablation Techniques
Radiofrequency ablation, laser ablation, and ethanol ablation can be used to treat small localized recurrences in the neck if someone is not a good candidate for surgery or if the tumor is in a difficult spot.
In some cases, these less invasive methods can be as effective as surgery for carefully selected patients.
Mental Health Resources
Mental Health Resources for Patients
Physicians are often eager to discuss the medical aspect of thyroid cancer, but may be less available to help you cope with the stress and mental toll this disease can have.
There are many questions worth asking about stress management, emotional wellness, and how both can impact a patient during the cancer journey.
This is not always the easiest conversation to start with a doctor, so we’ve provided resources to help you get questions about your emotional needs answered.
In order to keep your mental health in check, it’s important to be aware of signs, which can be subtle, that there is something affecting your mind. These signs might include:
- A change in eating or sleeping habits
- Losing interest in people or usual activities
- Experiencing little or no energy
- Numb and/or hopeless feelings
- Turning to drinking or drugs more than usual
- Non-typical angry, upset, or on-edge feelings
- Yelling/fighting with loved ones
- Experiencing mood swings
- Intrusive thoughts
- Trouble getting through daily tasks
These symptoms can be wide-ranging and vary a great deal from person to person. Everyone experiences grief differently, for example. However, if you are feeling unusually sad, on-edge, or like you’re no longer interested in activities you used to love, know that there are many treatment options available and many different healthy ways to help you cope.
Treatment options for people struggling with mental health really run the gamut. While some people may benefit from seeking the help of a psychologist and getting on medication, others see great improvement by simply implementing some lifestyle changes, such as prioritizing exercise and cutting back on alcohol.
Those struggling should know that they are not alone — about one in five American adults has experienced some sort of mental health issue, according to mentalhealth.gov. However, what worked to help someone else cope may not necessarily help you as treatment must be individualized.
+ Expand and Learn More...
To maintain a positive mindset and address mental health struggles you may be having, treatment may include:
- Seeking professional help from a psychiatrist or therapist
- Learning healthy coping skills
- Medication such as antidepressants
- Adding more physical activity to your routine
- Adjusting your sleep schedule
- Connecting with others via support groups
- Mindfulness and meditation
Integrative Medicine
Integrative Medicine to Help You Cope
Integrative medicine can be really helpful both during and after thyroid cancer treatment as a way to mitigate certain side effects. Integrative medicine doesn’t seek to replace traditional treatments, but aims to pair them with holistic methods of healing.
These days, many cancer doctors support integrating other methods into patient care. Integrative methods blend things like diet and stress management with conventional medicine. This includes things like acupuncture, meditation, or even medical marijuana to ease pain and other side effects.
Both the American Society of Clinical Oncology (ASCO) and the Society of Integrative Oncology (SIO) recommend meditation as part of a multidisciplinary approach to reduce stress, depression, and mood disturbance, and to improve the quality of life in cancer patients. That same approach can be beneficial during any hardship.
+ 5 tips for Practicing Mindfulness
5 tips for Practicing Mindfulness
- Choose one daily activity to practice mindfully (e.g. eating your lunch, brushing your teeth or taking a shower). During this activity notice your breath and activity of your mind for a few moments.
- Take a pause throughout your day. During your day, find a moment to stop and take five deep breaths with your eyes closed.
- Kindly acknowledge a moment you’re experiencing a difficulty by putting your hand on your heart and saying, “I feel my pain. How can I be kind to myself in this moment?”
- Get curious about your emotions. Experiment with welcoming your emotions as they come, instead of pushing them away.
- Become aware when you’re in a rush. Ask yourself, “Do I really need to hurry?”
Jon Kabat Zinn, founder of the eight-week stress-reduction program, Mindfulness-Based Stress Reduction (MBSR), a course that has entered the mainstream of health care, scientific study, and public policy, describes mindfulness as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally.”
The first step to being able to pay attention in the present moment is slowing down the mind often referred to as the “monkey mind.” This is done through a regular meditation practice.
The benefits of meditation can include increased calm, enhanced sleep quality, more energy, less physical pain, and increased well-being.
Living With Cancer
Diet, Exercise & Lifestyle
Living with advanced thyroid cancer can certainly manifest a mix of emotions and obstacles.
Perhaps one of the biggest obstacles you’ll have to deal with is cancer treatment and learning to cope with a new normal, as well as potential side effects. While everyone has their own journey with cancer treatment, experts have some golden rules to follow that are effective for getting through it.
+ Expand and Learn More...
Based on years of experience, Dr. Geoffrey Oxnard, a thoracic oncologist at Boston Medical Center, says he has a simple set of rules he tells his patients to help them cope.
- Don’t act sick: Just because you have cancer doesn’t mean that you have to stop doing the things that you enjoy. Stay active.
- Don’t lose weight: Cancer can eat away at your physical reserves, so it’s important that you top them up with the calories and nutrients you need to fight the disease.
- Don’t be a tough guy: When you have cancer, things like diarrhea or tingling nerves can be a sign that the dose or frequency of your treatment needs to be adjusted. Speak up and let the members of your care team know so that they can help.
Ultimately, dealing with your cancer treatment means staying positive, having full communication with those who can help and support you, and remembering that your life went on before treatment, and can go on just the same after treatment. There’s no reason why it shouldn’t go on during treatment.
And yes, you have the strength!

Please confirm you are a US based health care provider:
Yes, I am a health care Provider No, I am not a health care providerSign Up Now.
Take Control of Your Disease Journey.
Sign up now for expert patient guides, personalized treatment options, and cutting-edge insights that can help you push for the best care plan.