Jude Blume Beat Breast and Cervical Cancers
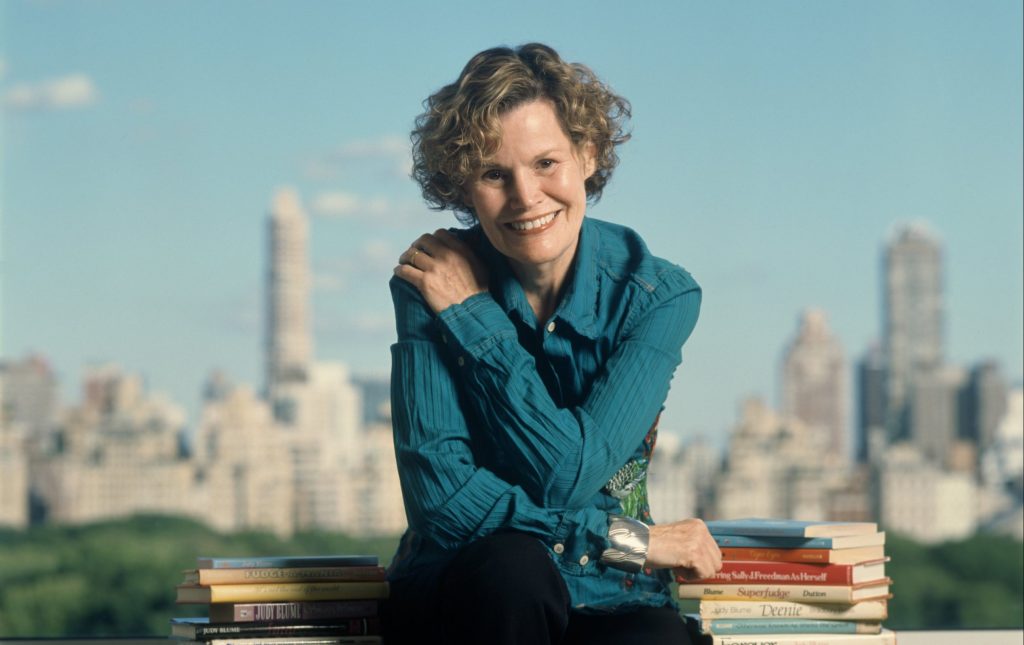
- Novelist Judy Blume, who battled early-stage breast cancer and cervical cancer, is celebrating the success of a Netflix series inspired by her book “Forever.”
- Stage zero breast cancer refers to DCIS otherwise known as Ductal Carcinoma In Situ. DCIS are abnormal cells that line the duct in a breast. A normal breast comprises lots of ducts (these ducts carry milk to the nipple in a woman who is lactating).
- Cervical cancer begins in the cells lining the cervix, the lower part of the womb (uterus). It usually develops slowly, however, before cancer presents itself. Vaginal bleeding or pelvic pains are common symptoms.
- Pap smears are one way to detect cervical cancer early. During the test, a doctor will collect a sample of cells from your cervix (using a small brush or spatula). The cells are then examined under a microscope for abnormalities, including cancer and changes that could indicate pre-cancer.
- It’s important to note that more than 70% of cases of cervical cancer are caused by the human papillomavirus (HPV). More than 90% of HPV-related cancers, including cervical cancer, are preventable in people who get the HPV vaccine that is recommended for all preteens (both girls and boys) 11 to 12 years old.
The New York University graduate—who has published 29 books, and the majority of those being novels for children, young adults, and adults—took to social media to announce share the good news from her bookstore in Key West, Florida.
Read MoreFans were quick to praise Blume, who previously fought early-stage breast cancer and cervical cancer, with support, with one writing, “Thank you Judy Blume for your permission to allow this adaptation to be made. It is such an important watch.”
Another fan commented, “I grew up on Judy Blume and as a grown woman fell in love with everything Mara Brock Akil has done, so this collaboration has given me LIFE!”
“So wonderful that this book is reaching a new generation in this new way!” commented a third.
A fourth wrote, “Oh I love these ladies as they are so very talented! Miss Blume is one of my reasons for loving reading, she writes the kind of novels that puts you right in the book as you’re reading it. Mrs. Brock-Akil is a phenomenal writer and producer, when these two were put together they created some serious literary magic.”
Back on May 7, Blume reminded her social media followers that Netflix’s eight-episode coming-of-age teen romance series “Forever” was debuting on May 8.
Blume, whose groundbreaking 1975 novel inspired the series, explained on Facebook, alongside footage of official teaser of the series, “Woo Hoo! Forever debuts on Netflix tomorrow May 8.
“It’s inspired by my novel, reimagined by Mara Brock Akil. I’ve seen all 8 episodes and hope you’ll enjoy it as much as I did. (A big plus for me was getting to know these parents.) Congrats to Mara, her team, and the cast.”
In a description about the show, Netflix explains, “Reunited as teens, two childhood friends fall deeply in love, experiencing the joy and heartache of a first romance that will change their lives forever.”
Judy Blume’s Cancer Battles
In September 2012, Judy Blume opened up in a blog post about her personal journey with cancer, detailing both her breast cancer diagnosis and her previous struggle with cervical cancer.
She had originally planned to spend the summer of 2012 in Italy, partially to work on completing her book “A Castle!” However, those plans took an unexpected turn after a routine breast screening in June.
“On June 12, during a standard ultrasound due to my dense breast tissue, the radiologist recommended a core biopsy,” Blume recalled.
The results confirmed she had ductal carcinoma in situ — an early form of breast cancer often referred to as stage 0.
Expert Resources On Stage Zero Breast Cancer
Her reaction was one of disbelief. “Breast cancer? Me?” she said.
“I don’t have a family history. I haven’t eaten red meat in over three decades. I’ve never smoked, I work out daily, I avoid alcohol because of my reflux, and my weight has stayed consistent my whole adult life. How could this be happening?” Blume wrote, expressing her surprise and confusion.
Once Blume came to terms with her diagnosis, she shifted her focus to finding the right treatment plan.
“Taking control—or at least feeling like I was—really helped me cope,” she shared.
After meeting with a couple of trusted doctors, she uldecided that a mastectomy followed by breast reconstruction was the right choice for her.
“The idea of a mastectomy wasn’t something I struggled with emotionally,” Blume explained. “Maybe because I’ve never felt like my breasts were tied to my identity or sexuality.”
When it comes to choosing a treatment path, especially surgery, every woman’s situation is different. Some may consider breast-conserving options like a lumpectomy, and that choice often depends on open, honest conversations with your doctor. It’s all about weighing the risks and benefits together.
Things like the size of the tumor, its specific characteristics, and your family history can all play a role in deciding whether a mastectomy is the best option. And if you do decide to have both breasts removed, the emotional weight of that decision can feel especially significant.
WATCH: Regaining your sense of self after reconstruction.
Some women decide to have their breasts reconstructed and have implants put in right after the mastectomy, while others don’t have reconstruction at all.
Dr. Elisa Port is a surgeon who specializes in the care and treatment of patients with breast cancer at Mount Sinai Health System. She added that most women opt to have some reconstruction. The length of these surgeries can vary greatly. When implants are used, the procedure can take two to three hours (so the total surgery time would be around five hours). There is also the option to take one’s own tissue (usually from the belly area) and transfer it into the breast area during reconstruction.
“When it comes to reconstruction, there are more decisions to make – implants or autologous? If implants, saline or silicone? By then, I was so tired of having to make decisions I went with whatever would make the surgery easiest on me,” Blume said.
Blume’s Cervical Cancer Diagnosis, Linked To HPV
Blume also said that she was diagnosed with cervical cancer, which was caused by the human papillomavirus (HPV), in 1995. She chose to undergo a hysterectomy for treatment.
“We didn’t know it was cervical cancer before the surgery, but we knew something was going on. Caught it just in time, extensive but still in situ (very early stages).” Blume explained.
Cervical cancer begins in the cells lining the cervix, the lower part of the womb (uterus). It usually develops slowly, however, before cancer presents itself. Vaginal bleeding or pelvic pain are common symptoms.
Cervical cancer, which has been linked to the human papillomavirus (HPV), is curable when discovered early through routine screening, which is done through Pap Smears or HPV tests. A pap smear can be used to detect cervical cancer or changes in cervical cells that suggest a woman is at risk of developing cervical cancer.
Blume credits her family and friends who offered her support while undergoing cancer treatment.
What to Know About Screening For Breast Cancer
The medical community has a consensus that women between 45 and 54 have annual mammograms. However, an independent panel of experts called the U.S. Preventive Services Task Force (USPSTF) is saying that women should start getting mammograms every other year at the age of 40, suggesting that this lowered the age for breast cancer screening could save 19% more lives.
WATCH: Screening for Breast Cancer
For women aged 55 and older, the American Cancer Society recommends getting a mammogram every other year. However, women in this age group who want added reassurance can still get annual mammograms.
Women who have a strong family history of breast cancer, have dense breasts, have a genetic mutation known to increase the risk of breast cancer, such as a BRCA gene mutation, or a medical history, including chest radiation therapy before age 30, are considered at higher risk for breast cancer.
Understanding the BRCA Gene Mutation
Experiencing menstruation at an early age (before 12) or having dense breasts can also put you into a high-risk category. If you are at a higher risk for developing breast cancer, you should begin screening earlier.
Breast density is determined through mammograms. However, women with dense breasts are at a higher risk for developing breast cancer because dense breast tissue can mask potential cancer during screening. 3D mammograms, breast ultrasound, breast MRI, and molecular breast imaging are options for women with dense breasts for a more precise screening. It is important to ask your doctor about your breast density and cancer risk.
Although breast cancer can happen to anyone, certain factors can increase a person’s risk of getting the disease. The known risk factors for breast cancer include:
- Older age
- Having a gene mutation such as the BRCA1 or BRCA2
- Added exposure to estrogen
- Having children after the age of 30
- Exposure to radiation early in life
- Family history of the disease
RELATED: Is Genetic Testing Right for You?
Different types of genetic testing can help people with a family history of cancer better ascertain their cancer risks. Your doctor will discuss your family history of cancer with you in the context of your type of tumor and your age at diagnosis. Hereditary genetic testing is usually done with a blood or saliva test.
The second test involves the genetic sequencing of your tumor if you’ve been diagnosed with cancer by this point. These genetic changes can be inherited, but most arise during a person’s lifetime. This process usually involves examining a biopsy or surgical specimen of your tumor. This testing can lead to decisions on drugs that might work against your cancer.
WATCH: Understanding genetic testing for breast cancer.
About ten percent of breast cancers are hereditary, says Dr. Ophira Ginsburg, Director of the High-Risk Cancer Program at NYU Langone’s Perlmutter Cancer Center.
“We encourage only those who have a family history to really get [genetic testing],” Dr. Ginsburg previously told SurvivorNet.
“I would say that if you have anyone in your family who was diagnosed with a very rare cancer. Or if you have a strong family history of one or two kinds of cancer, particularly breast and ovarian, but also colon, rectal, uterine, and ovarian cancer, that goes together in another cancer syndrome called the Lynch Syndrome,” Dr. Ginsburg adds.
When You’re Getting a Mammogram, Ask About Dense Breasts
Understanding Cervical Cancer & Pap Smears
Cervical cancer begins in the cells lining the cervix the lower part of the womb (uterus). Treatment options for cervical cancer include surgery, chemotherapy and/or radiation therapy.
It’s important to note that HPV (human papillomavirus), a sexually-transmitted virus, causes more than 70% of cervical cancer cases. Most cases of cervical cancer can be prevented with the HPV vaccine.
Additionally, other risk factors like smoking can make you about twice as likely to get cervical cancer as those who don’t smoke.
Cervical cancer screening is critically important because an earlier diagnosis can mean a better prognosis with broader treatment options.
The American Cancer Society recommends that cervical cancer screening begins at age 25, and people aged 25 to 65 should have a primary HPV test, an HPV test done by itself for screening, every five years. If primary HPV testing is not available, however, screening may be done with either a co-test that combines an HPV test with a Papanicolaou (Pap) test every five years or a Pap test alone every three years.
The most common symptoms of cervical cancer include:
- Abnormal vaginal bleeding, such as bleeding after vaginal sex, bleeding after menopause, after douching, bleeding and spotting in between periods or having heavier or longer (menstrual) periods than usual
- Unusual discharge from the vagina that may contain some blood and may occur between your periods or after menopause
- Pain during sex
- Pain in the pelvic region
Pap smears are one way to detect cervical cancer early. During the test, a doctor will collect a sample of cells from your cervix (using a small brush or spatula). The cells are then examined under a microscope for abnormalities, including cancer and changes that could indicate pre-cancer.
This is an important procedure because symptoms of cervical cancer might show up until the disease is at stage 3 or 4. By helping doctors catch signs of the disease early, Pap smears can lead to broader and more effective treatment options.
One of the leading causes of cervical cancer is the human papillomavirus (HPV), one of the most common viruses which can be transmitted through sexual contact. HPV is the biggest risk factor for cervical cancer, and there are usually no early signs or symptoms of the disease. However, cervical cancer can be detected through regular check-ups, such as pap smears.
According to the Centers for Disease Control and Prevention, it’s recommended that women start getting Pap tests at age 21. “If your Pap test result is normal, your doctor may tell you that you can wait three years until your next Pap test,” the CDC explains.
Meanwhile, anyone between 20 and 65 years old is urged to speak with their doctor on which testing option is best for them. The CDC explains, “An HPV test only. This is called primary HPV testing. If your result is normal, your doctor may tell you that you can wait five years until your next screening test.
“An HPV test along with the Pap test. This is called co-testing. If both of your results are normal, your doctor may tell you that you can wait five years until your next screening test. A Pap test only. If your result is normal, your doctor may tell you that you can wait three years until your next Pap test.”
For women older than age 65, the CDC says your doctor may suggest you don’t need further screenings if: “You have had at least three Pap tests or two HPV tests in the past 10 years, and the test results were normal or negative, and you have not had a cervical precancer in the past, or you have had your cervix removed as part of a total hysterectomy for non-cancerous conditions, like fibroids.”
The Importance of Routine Screenings For Cervical Cancer
Regular cervical cancer screenings play a vital role in the early detection and prevention of cervical cancer. SurvivorNet experts explain that timely cervical cancer screenings are essential because they:
- Help identify abnormal cells early: Screenings can detect abnormal cervical cells (also called cervical dysplasia) before they turn into cancer. Early detection allows for timely interventions and treatment, preventing the progression to cervical cancer.
- Reduce the risk of cervical cancer: Consistent and regular screenings have been shown to significantly decrease the risk of developing cervical cancer. The more often you get screened, the higher the chance of catching any abnormal cells early enough to treat them effectively.
- Confidence in your health status: Regular screenings provide peace of mind, knowing you’re taking steps to safeguard your health. Whenever abnormal cells are detected and treated, it helps maintain your overall well-being and offers reassurance.
Despite the benefits of regular screenings, some people may neglect them due to factors such as a lack of awareness, fear, or procrastination. It’s essential to remember that both the Pap test and HPV test usually take only a few minutes, easily performable during a regular doctor’s visit. The best preventative measure against cervical cancer is attending regular screenings and updating your healthcare provider on any changes in your gynecological health.
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

