Life After Cancer and the Fear of Its Return
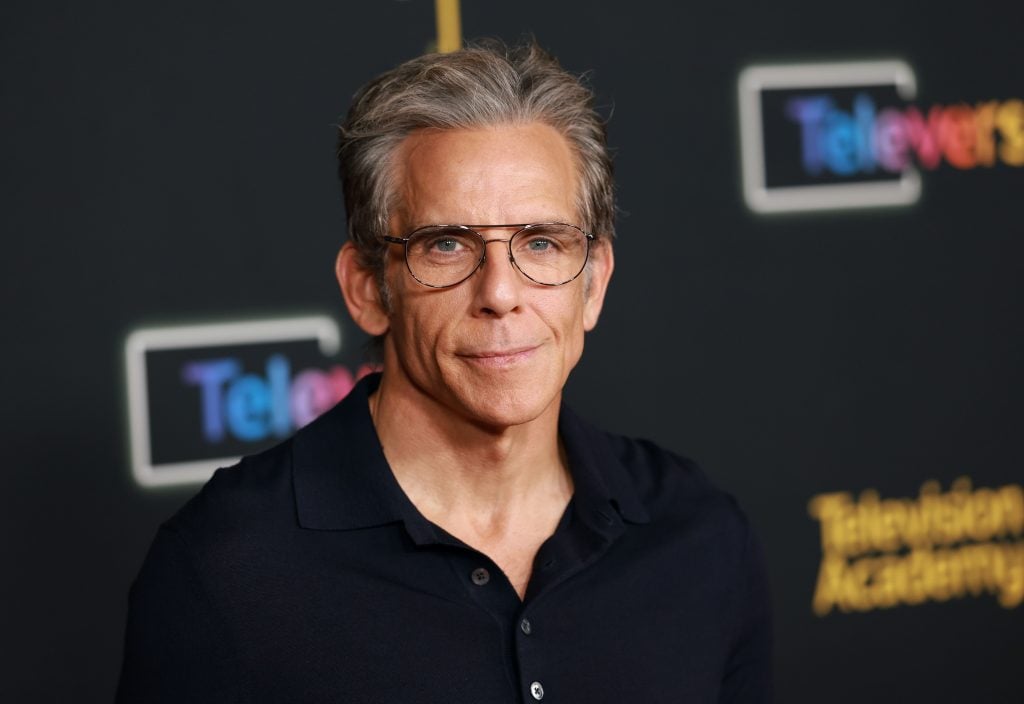
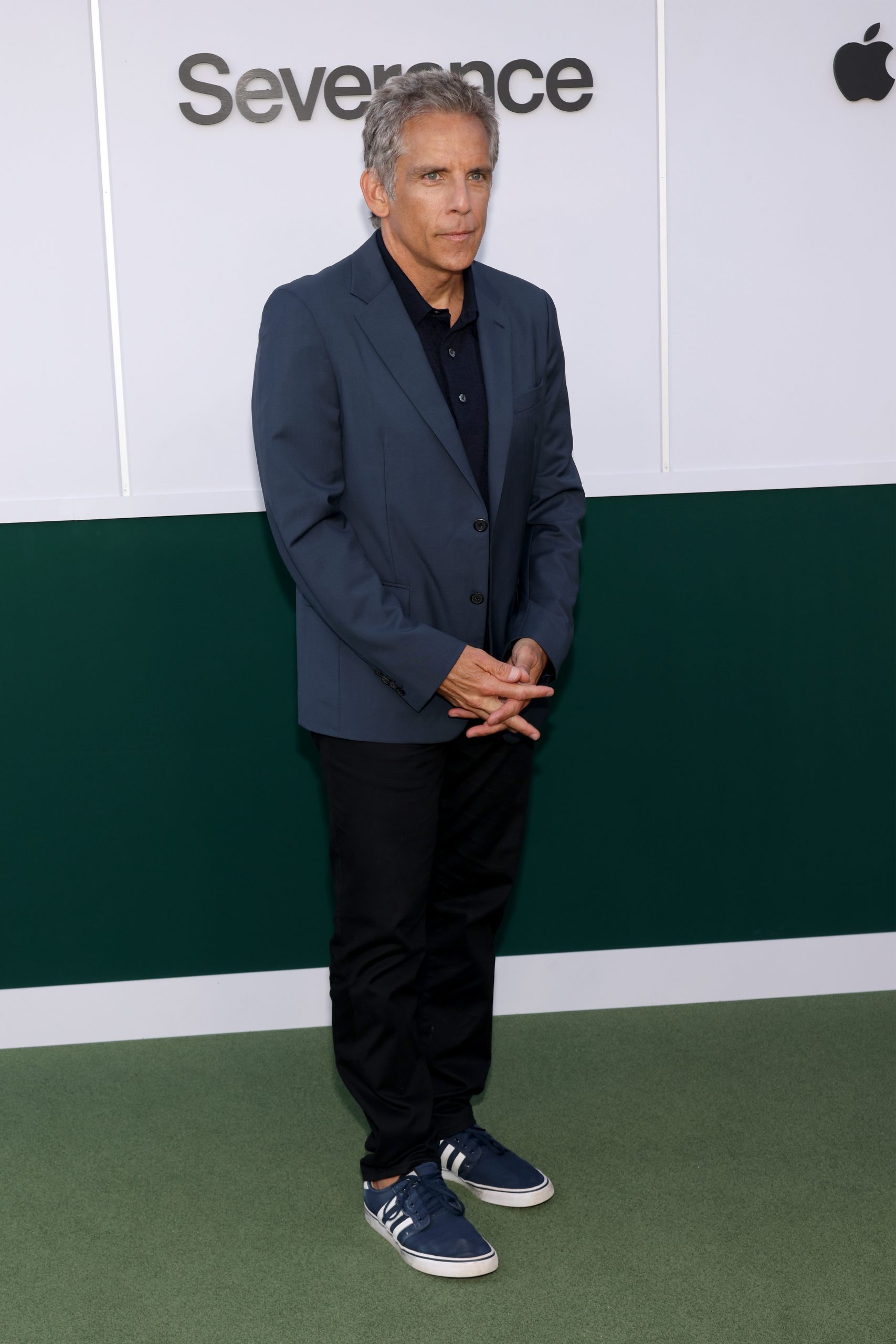
- Ben Stiller, 59, may have been declared cancer-free more than a decade ago, but the emotional imprint of his prostate cancer diagnosis still lingers. The actor-turned-producer admits that the fear of recurrence continues to shadow his sense of relief—a sentiment shared by many survivors and often overlooked in public narratives about recovery.
- Stiller was diagnosed with prostate cancer in 2014 after undergoing a prostate-specific antigen (PSA) test. The test measures the prostate-specific antigen in the blood.
- An elevated PSA level in the blood does not always mean you have prostate cancer, but it calls for further testing.
- Stiller underwent a prostatectomy, which is a surgical treatment option for men with any risk group of prostate cancer that hasn’t spread outside of the prostate gland.
- During this procedure, the surgeon removes the entire prostate, along with some tissue around it, including the seminal vesicles that release fluid into the semen. Side effects may follow this procedure, which may include erectile dysfunction and urinary incontinence.
“[Prostate cancer] It’s scary because all of a sudden it’s like boom, stop because you don’t know if you’re going to be alive in six months if this doesn’t get dealt with,” Stiller shared during a candid conversation on The Prof G Pod with Scott Galloway.
“The movie just tanked, but it was, literally to this day, my favorite experience ever making a movie,” he said.
But the conversation took a deeper turn when Stiller opened up about his health journey—a diagnosis that would change everything.
“I had a bad diagnosis in terms of my doctor wasn’t great at what he told me. PSA test, and you have to watch it,” he explained. “My doctor started testing me early because he saw it growing. Then you do a biopsy when they see something spiking up there, which is scary.”
The initial shock led Stiller to seek a second opinion, where he found a more compassionate and proactive approach.

“The new doctor laid it out and said you’ve got to do this operation, and that was ten years ago, and I’m cancer-free,” he said.
Still, the relief of remission hasn’t erased the fear. Stiller admits that the experience left a lasting imprint.
“I do worry going forward, because just because you’ve had cancer once, it isn’t like you can’t get cancer again,” he said.
Stiller’s story is a powerful reminder of the importance of early detection, self-advocacy, and the emotional complexity of survivorship—even years after treatment ends, the worries do not end as quickly.
Helping Patients Understand Prostate Cancer Treatment Options
How Stiller Coped With Cancer
When Stiller was diagnosed, he happened to get a prostate-specific antigen test (PSA), which measures the prostate-specific antigen in the blood. An elevated PSA level in the blood does not always mean you have prostate cancer, but it does call for further tests. The “Zoolander” also underwent a biopsy, which revealed he had “mid-range aggressive” cancer.
Since he was at higher risk, Stiller had a prostatectomy. This procedure is an option for men with any risk group of prostate cancer that hasn’t spread outside of the prostate gland.
During the procedure, the surgeon removes the entire prostate, along with some tissue around it, including the seminal vesicles that release fluid into the semen. Side effects may follow this procedure, which may include erectile dysfunction and urinary incontinence.
However, how long these side effects may linger is what the CEASAR (Comparative Effectiveness Analysis of Surgery and Radiation for Localized Prostate Cancer) study, coordinated by Vanderbilt University Medical Center, sought to answer.

The study followed roughly 2,500 men from diverse backgrounds in the United States. All of the men were diagnosed between 2011 and 2012 with prostate cancer and had received treatment.
Over ten years, the participants were closely monitored and asked to answer several questions regarding side effects related to urinary, bowel, sexual, and hormone therapy.
The participants were placed into two groups depending on their treatment plan. One group included patients treated with active surveillance, nerve-sparing prostatectomy, external beam radiation therapy (EBRT), and low-dose-rate brachytherapy.
Active surveillance is a “watch-and-wait” approach for men with low-risk prostate cancer, meaning you have a small number of cancer cells found in your biopsy, a low PSA, and a low-grade cancer. This approach is typically enough for men with low-risk prostate cancer. However, if you’ve been diagnosed with moderate-risk cancer, more may be needed.
WATCH: Understanding How Active Surveillance Works
Nerve-sparing prostatectomy surgically removes the prostate while protecting the nerves to minimize the side effects of erectile dysfunction. External beam radiation therapy uses high doses of radiation to stop cancer cells from dividing and shrinking tumors. Low-dose-rate brachytherapy is a form of radiotherapy.
The second group of study participants was treated with prostatectomy or external beam radiation therapy with androgen deprivation therapy (ADT), which combines radiation treatment with anti-hormone therapy, which reduces the male hormone androgen.
The study’s findings suggest that for “Men with localized prostate cancer (cancer confined to the prostate), radical prostatectomy was associated with a greater decrease in sexual function and urinary incontinence than either EBRT or active surveillance after three years and was associated with fewer urinary irritative symptoms than active surveillance.”
“However, no meaningful differences existed in either bowel or hormonal function beyond 12 months or in other domains of health-related quality of life measures.”
Managing Prostate Cancer & Treatment Side Effects
For men with localized prostate cancer, radical prostatectomy was associated with “significant declines in sexual function” compared with EBRT and active surveillance. Urinary incontinence scores by participants also “declined significantly after surgery compared with EBRT and active surveillance.”
WATCH: A Healthy Sex Life Is Possible After Prostate Cancer
In addition to gauging possible long-term side effects of certain prostate cancer treatments, researchers say they hope their findings help patients and their care team fine-tune their treatment outlook.
“The findings underscore the importance of counseling men with unfavorable prognosis prostate cancer differently than favorable prognosis cancer regarding expected long-term functional outcomes and suggest that adverse effects of treatments on sexual function may be deemphasized in decision making for some men,” senior author Dr. Daniel Barocas professor and executive vice chair of Urology at Vanderbilt University Medical Center (VUMC) told the VUCM Reporter.
Questions for Your Doctor
If you have experienced symptoms associated with prostate cancer or have a screening coming up, here are some questions you may ask your doctor:
- If I had elevated PSA levels, what could be causing that besides cancer?
- How long will it take to learn if my PSA levels warrant further testing?
- What are the treatment options that are best suited for me based on my risk level?
- What financial resources exist to help me with the costs associated with treatment?
- How long will my potential treatment prevent me from working or continuing normal activities?
Learn more about SurvivorNet's rigorous medical review process.

