Living With Brain Cancer Doesn't Mean You Can't Focus On Things That Bring You Joy In Life
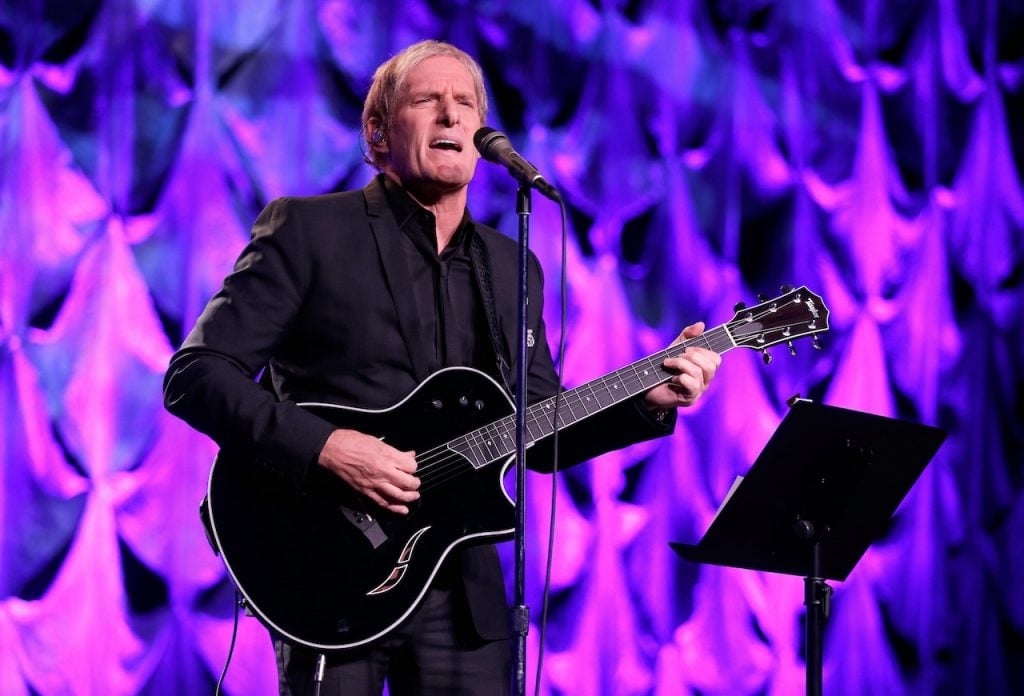
- Singer Michael Bolton, 72, grows nostalgic for a long-standing performance venue that helped kickstart his career many years ago. A bright spot in his life is that he lives with glioblastoma, an aggressive form of brain cancer.
- Bolton’s diagnosis emerged after suffering from symptoms including difficulty with his balance, memory, and headaches. He underwent brain surgery to remove the tumor and received chemotherapy and radiation afterward to complete his treatment. As of Spring 2025, his scans returned clear, although glioblastomas have a tendency to come back after treatment.
- Grade IV gliomas – These are the most aggressive gliomas, which are locally aggressive and require treatment intensification. Glioblastomas are the most common grade IV glioma, “which is by far the most well-known and feared tumor in the lay population and, quite frankly, the medical population,” Dr. Henry Friedman, renowned brain cancer expert, explained to SurvivorNet.
- To treat a brain tumor, doctors can perform a craniotomy — a surgical procedure where doctors remove part of the skull and resect the tumor. This option is typically pursued when the tumor causes symptoms like seizures, headaches, or neurological impairment.
- The primary goal of brain tumor surgery is to safely remove as much of the tumor as possible while preserving essential brain functions. However, some tumors are located in delicate or inaccessible areas, making full resection difficult.
- Following surgery, patients often undergo radiation and chemotherapy to help eliminate remaining cancer cells that couldn’t be removed during the procedure.
- Even after aggressive treatment, the risk of tumor recurrence, meaning the tumor can return, remains. Long-term care strategies focus on monitoring and managing this persistent threat with ongoing therapy and support.
In the midst of treatment and recovery, Bolton paused to honor a venue that helped launch his career.
View this post on Instagram
Bolton’s symptoms began subtly: headaches, loss of balance, and a sudden fall that alarmed his family.
“He fell out of his chair to the left, which is very unusual. He’s super athletic, and he doesn’t drink,” she added. “So he fell, and we were like, ‘What just happened?’” Bolton’s daughter previously shared with People Magazine.

An MRI revealed a brain tumor that doctors later confirmed was glioblastoma.
Glioblastoma (GBM) is an aggressive form of brain cancer. It grows and spreads very quickly. Patients typically have an average survival rate of 15 months with treatment and less than six months if left untreated.
Bolton underwent emergency surgery in December 2023. Remarkably, doctors were able to remove the tumor entirely—a rare outcome in glioblastoma cases, where microscopic remnants often remain after surgery. However, Bolton’s journey didn’t end there. A post-surgical infection led to a second brain surgery in early 2024, followed by months of radiation and chemotherapy.
View this post on Instagram
Glioblastoma has a recurrence rate nearing 90% and a progression-free survival average of just seven months. Research published in the peer-reviewed research journal “Cancers” says that glioblastoma is “one of the most aggressive tumors, and recurrence is almost unavoidable. The mean progression-free survival (PFS) is approximately 7 months since diagnosis.”
Bolton’s care team continues to monitor his health with regular MRI scans. As of spring 2025, his scans have returned clear—no signs of disease progression.

Throughout it all, Bolton has leaned on his daughters, grandchildren, and fans for strength.
“Sharing such a profoundly personal chapter of my life hasn’t been easy,” Bolton said in an Instagram post while speaking out about his brain cancer journey.
“My hope in sharing this part of my journey is that it might offer comfort to other families facing similar challenges, and perhaps even inspire those navigating their own adversity,” Bolton said.
Helping Patients Better Understand Brain Cancer
Understanding Bolton’s Glioblastoma Diagnosis
Diagnosing gliomas involves a multi-step approach that includes clinical assessment, imaging studies, histopathological examination, and molecular testing.
As patients are diagnosed, they’re observed for typical glioma symptoms. These may include:
- Headaches
- Seizures
- Cognitive or Behavioral Changes
- Visual or Speech Changes and Impairments
- Loss of Body Weight and Deconditioning
- Changes in mental function, mood, or personality
- Changes in speech
- Sensory changes in hearing, smell, and sight
- Loss of balance
- Changes in your pulse and breathing rate
During the clinical assessment, the physician will take a detailed history, focusing on the onset and progression of symptoms. Since gliomas can present with non-specific symptoms that overlap with other neurological conditions, ruling out conditions like stroke, infections, or inflammatory disorders is essential during the initial clinical evaluation.
Patients then undergo a neurological exam that tests cranial nerve function, motor strength and coordination, sensory function, and cognitive abilities.
Next, patients undergo an MRI, which provides doctors with a visualization of the tumor.
“If you’re suspected of having a tumor on imaging and our neurosurgeons think that tumor can come out, they will take a piece of that tumor out first and confirm in the operating room and with our pathologists that, in fact, what they are looking at is a tumor,” Dr. Alexandra Miller, Director of the Neuro-Oncologist Division at NYU Langone Health, tells SurvivorNet. “And if it is, they resect it at that time. It’s not usually a two-step procedure.”
If surgery cannot be performed due to tumor location or patient-specific factors, a less invasive stereotactic biopsy can be obtained. Once the tissue sample is obtained, it’s examined under a microscope for molecular testing. At this stage, the tumor is given a grade, which determines how aggressive it is.
- Grade I-II gliomas – These are considered low-grade and tend to grow slowly. “The grade one is a very indolent, benign tumor that can be cured with surgery alone,” Dr. Henry Friedman, Deputy Director of the Preston Robert Tisch Brain Tumor Center at Duke, tells SurvivorNet.
- Grade III gliomas—These are considered high-grade and tend to grow more rapidly. They are typically classified as malignant and require more aggressive treatment, which can include surgery, radiation, and chemotherapy.
- Grade IV gliomas – These are the most aggressive gliomas, which are locally aggressive and require treatment intensification. Glioblastomas are the most common grade IV glioma, “which is by far the most well-known and feared tumor in the lay population and, quite frankly, the medical population,” Dr. Friedman explains.
Inside Brain Tumor Surgery and Recovery: What Patients Can Expect
Surgery to remove a brain tumor is delicate by nature, and every movement inside the skull must balance precision with safety.
“We take off the bone overlaying the area we need to get to. We open the little envelope around the brain called the dura, and then we move through the brain tissue to get to where the tumor is to try to cut out as much as we can safely—without hurting the patient’s function or other important things like big blood vessels that can cause things like a stroke,” explains Dr. Kimberly Hoang, a board-certified neurosurgeon at Emory University School of Medicine.
Following surgery, patients are closely monitored and often receive radiation to prevent tumor regrowth—particularly in cases where multiple tumors or metastatic disease are involved.
“Because many patients can have more than one brain tumor or metastasis from their cancer, it was not reasonable to think about surgery for them,” Dr. Hoang adds. “They also get radiation for those spots as well, to try to keep those tumors from growing or shrink them down.”
Treatment Advancements & the Challenge of the Blood-Brain Barrier
Chemotherapy, immunotherapy, and targeted therapies have long been effective in treating cancer throughout the body. But the brain’s natural defense — the blood-brain barrier — makes these treatments less effective when it comes to brain tumors.
This barrier is “a network of blood vessels and tissue…made up of closely spaced cells and helps keep harmful substances from reaching the brain,” according to the National Cancer Institute.
Still, Dr. Hoang notes that recent advancements in drug design are beginning to improve treatment efficacy in the brain.
Understanding Side Effects of Brain Tumor Treatment
Side effects vary depending on the tumor’s size, location, and number of lesions present.
“Radiation treatment can cause swelling in the tumor as the tumor ‘dies,’ and the surrounding tissue can also become swollen as the treatment takes effect,” Dr. Krishanthan Vigneswaran, a neurosurgeon with UT Health Houston and Memorial Hermann, tells SurvivorNet.
“This swelling can cause symptoms of headache, nausea, vomiting, and neurological loss of function…Surgical resection can also induce swelling, but this is more transient.”
Tumor location often determines what symptoms emerge:
“If it’s near your movement area, movement on one side of the body can be affected. If it’s near your speech area, your speech and the way you form words and express them can be affected,” Dr. Hoang explains.
She also notes brain surgery tends to be less painful than other types — like spinal or abdominal — due to fewer nerves in the surgical area.
Recovery & Long-Term Monitoring
Simpson still receives recurring MRI scans to monitor his brain for any signs of cancer progression.
“Because of this unique quality of metastatic brain disease, an oncology team will have to monitor a patient indefinitely during remission,” Dr. Vigneswaran says.
Many experts recommend joining a support group — especially one with people who’ve undergone similar procedures. Their lived experience can offer comfort and practical advice.
“Support groups can be incredibly helpful to patients and are commonly offered at major cancer centers and hospitals,” says Dr. Jennifer Moliterno, Chief of Neurosurgical Oncology at Yale Cancer Center.
Mental health professionals are also often part of the care team, helping patients manage the emotional effects of surgery, treatment, and recovery.
Current Options to Treat Glioblastoma
The Food and Drug Administration (FDA) has approved some drug treatments, including temozolomide (Temodar), to help patients living with this aggressive disease.
Temozolomide is a chemotherapy drug patients can take after surgery and radiation therapy.
Dr. Daniel Wahl, professor of radiation and oncology at the University of Michigan, explains Temozolomide is an oral drug that ” slows down tumor growth.”
“Patients with GBM have effective treatment options; there are four of them: surgery, radiation, chemotherapy, and tumor targeting fields. These are electric fields that we can use to treat these cancers,” Dr. Wahl said.
Other FDA-approved drugs for treating glioblastoma include lomustine (Gleostine), intravenous carmustine (Bicnu), carmustine wafer implants, and Avastin (bevacizumab).
Avastin is a targeted drug therapy that blocks glioblastoma cells from requesting new blood vessels that feed and allow the tumor to grow.
“Outcomes for these patients are still suboptimal. What I tell my patients is that we have these effective treatments, but what they do is they delay the time to when this tumor comes back. Only in exceptional circumstances would we ever talk about getting rid of one of these cancers, a few,” Dr. Wahl said.
WATCH: Using electric sources to improve glioblastoma treatment.
Fortunately, research is ongoing to improve the prognosis for people battling glioblastoma. One area of promise is tumor-treating fields, which can help extend patients’ lives by two years on average, giving them hope.
Optune, the brand name for the tumor-treating field delivery device, was launched in 2011 and approved by the FDA in 2015. It is a wearable and portable device for glioblastoma treatment for adult patients aged 22 years or older.
“There’s been a very exciting development of tumor treating fields, which are electrical fields that have been applied to the brain,” Dr. Suriya Jeyapalan, a neurologist at Tufts Medical Center, previously told Survivor Net.
TTFields use low-intensity electric fields to disrupt the cell division process, making it harder for cancerous cells to multiply.
Despite Optune’s hope, not all cancer experts agree with its approach, including Dr. Friedman.
“Although the National Comprehensive Cancer Network (NCCN) recognizes Optune within its guidelines as a therapy for glioblastoma, many people don’t believe it adds value. At Duke, for example, we don’t consider it a mainstay of therapy,” Dr. Friedman said.
Questions for Your Doctor
If you have been diagnosed with glioblastoma, here are some questions you may consider asking your doctor:
- What stage is my brain cancer?
- What are the treatment options for my brain cancer?
- Am I a good candidate for temozolomide?
- Am I a good candidate for Optune?
- What are the risks and benefits of the recommended treatment?
- What are the side effects of the recommended treatment?
- How long will it take to recover from treatment, and will I be able to return to work and normal activities?
- What’s the likelihood that insurance will cover the recommended treatment
Learn more about SurvivorNet's rigorous medical review process.

