Finding Purpose Amid a Major Health Challenge
- A stage 4 bone cancer patient who was diagnosed as a teen now works as a social worker, helping other patients battling health challenges and offering hope for brighter days ahead.
- Katelyn Tillman was diagnosed with an aggressive form of bone cancer called osteosarcoma, which grows and spreads rapidly. She’s undergone surgeries, including removing her leg and lung, and numerous stints of chemotherapy for treatment.
- One of the primary roles of a social worker is advocacy. Social workers help with a variety of issues that arise with cancer treatment. They can connect you with financial resources to help pay for treatment, work with insurance companies, and provide emotional support for those who need it.
- They can also help guide patients through the treatment process, including setting up appointments, getting them financial, legal, or other forms of support, setting up transportation, and more.
- A patient navigator can also help patients communicate with doctors, insurance companies, employers, lawyers, or others involved in medical care.
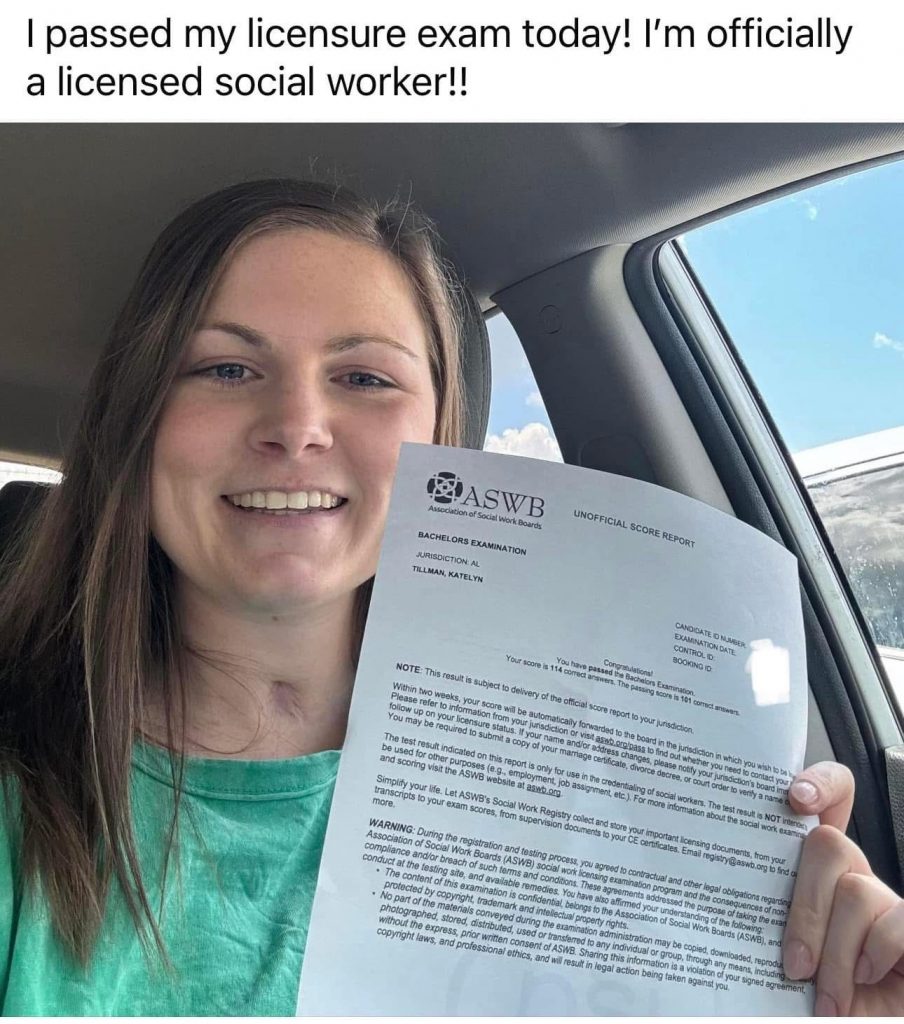
“We were very fortunate, and we had amazing social workers when we were in and out of the hospital. So that led me to want to be able to help people with the medical and the other stuff that’s affected,” Tillman told WKRG news.

“After being in the hospital and meeting social workers, I knew this is what I wanted to do,” Tillman added.
Tillman had her leg amputated during her bone cancer treatment. She also had her lung removed. Her cancer treatments included chemotherapy, which often leaves patients reeling with its grueling side effects.
“Probably one of the big [chemo side effects] is fatigue,” medical oncologist Dr. Marleen Meyers tells SurvivorNet.
“That’s a very common symptom, which goes with a lot of treatment for cancer,” Dr. Meyers adds.
The best way to manage chemotherapy side effects is to prepare for them. Gynecologic oncologist Dr. Matthew Carlson provides some examples of helpful ways to manage chemo side effects:
For nausea, doctors will usually prescribe effective medications, including Zofran. “We have many, many, many medications that we give before, during, and after chemotherapy that should minimize the nausea that patients experience,” Dr. Carlson says, adding that there are also quite a few medications available for constipation and diarrhea. However, doctors may recommend dietary modifications first.
While there aren’t quite medications for fatigue the way there are for nausea, Dr. Carlson says that some patients may find it helpful to complement their treatment with alternative medicine supplements such as American Ginseng.
WATCH: Managing Chemotherapy Side Effects
And then there’s the chemotherapy side effect everyone asks about: hair loss.
“When it comes to the hair loss associated with chemotherapy, we can’t keep you with a full head of hair through your chemotherapy,” says Dr. Carlson.
Wigs, scarves, caps, and cutting your hair short can all help, as can scalp-cooling devices, which can prevent some (though not all) hair loss. It’s important to remember that hair loss is usually temporary and typically regrows after treatment.
WATCH: Helping Dealing With Chemo Side Effects
“Sometimes it can be scary picturing what life will look like when you go home. It may not look the same, but I can encourage them that they can do this, and there is life outside the hospital,” Tillman said.
Tillman’s colleagues at USA Health Children’s and Women’s Hospital in Mobile, Alabama, say that she inspires patients and healthcare professionals at the hospital.
“Katelyn serves as an inspiration to those who are dealing with similar physical challenges or obstacles,” Nicoll Mastin, Director of Care Management, said.
“The most rewarding part of my job is being able to see children leave the hospital with their families. It’s very exciting to see a child recover and get to go home,” Tillman told USA Health.
Help With Navigating Cancer Treatment
How Patient Navigators and Social Workers Help
A patient navigator plays a crucial role in guiding individuals through the complex and often overwhelming cancer journey. From diagnosis and treatment to financial challenges and follow-up care, they provide essential support every step of the way.
When patients are juggling emotional distress and an influx of medical information, a patient navigator can be a lifeline—helping them access resources, coordinate care, and focus on healing.
“Patient navigators can function differently at different hospitals,” Dr. Kathie-Ann Joseph, a surgical oncologist at NYU Langone Health’s Perlmutter Cancer Center, told SurvivorNet.
“We have a really wonderful program at [NYU] where we used lay navigators, meaning they’re not nurses, although you can use nurses or social workers, that pretty much help newly diagnosed cancer patients through the continuum of care.”
These navigators can meet with patients from their first doctor’s appointments and can also:
- Attend appointments
- Provide an assessment for the next steps of care
- Assist with housing, transportation, or immigration issues
- Help with financial issues
- Provide direction on legal issues
“They really will help them get through these barriers that we think could impact their care,” Dr. Joseph added. “Because the goal is we want them to complete their care.”
Understanding Katelyn’s Bone Cancer Diagnosis
Tillman was diagnosed with osteosarcoma in 2014. This type of bone cancer is more aggressive and can spread quickly. For treatment, she began receiving chemotherapy. Then, she underwent surgery to remove the cancerous tumor in her leg, which was ultimately amputated in early 2015.
Her cancer progressed, reaching stage 4, and metastasized or spread to her lungs, resulting in a surgical procedure called a lobectomy, which removes a lung. Additional radiation and chemotherapy followed her lung surgery. After remaining in a coma for more than two months, she was able to go home. Continuing her education became a focus. After graduating college, she’s working on a degree in social work, using her experience as fuel.
Primary bone cancer means the cancer originates in the bone itself, and it is extremely rare—“less than one percent,” the National Cancer Institute says. Most bone cancer is a secondary cancer, meaning it originated elsewhere in the body.
The main types of primary bone cancers include:
- Osteosarcoma can grow quickly and spread to other parts of the body.
- Chondrosarcoma, which begins in the cartilage tissue.
- Ewing sarcoma is a fast-growing tumor that can spread to other parts of the body.
- Chordoma is a rare, slow-growing tumor. It is more likely to form in the spine.
People diagnosed with bone cancer may experience pain or swelling near a bone. However, not all bone cancers and tumors (benign and malignant) present symptoms.
Treatment options depend largely on specific details of the cancer and the patient’s overall health. However, surgery, chemotherapy, radiation, targeted therapy, and cryosurgery (freezes cancer cells to kill them) are common treatment methods.
Learn more about SurvivorNet's rigorous medical review process.

