Five days before her baby was due, photographer, Missy Peters was diagnosed with stage 2 breast cancer. "I felt a million miles from 'sick' and cancer wasn't anywhere on my radar," says Peters, who’d had a lump checked — and cleared — months before.
When her doctor said she was was “too young” for breast cancer, she believed him.
Read MoreWhile she was undergoing cancer treatment, Peters met other young women who, like her, had seen their symptoms dismissed due to their age. “I felt like I'd been duped by life or maybe just by statistics?” she told San Diego Voyager. To make matters worse, many had their diagnoses delayed after doctors said: "Let's see if it's still there in 6 months".
On her final day of chemo, Peters set up her tripod and snapped a self-portrait, “bald, holding my baby.” She shared the photo hoping other young women would read her story and begin doing a breast self-exams — and “The Breast Cancer Portrait Project” was born.
“I photograph young women diagnosed with breast cancer and share their stories to raise awareness that young women get breast cancer, too," says Peters.
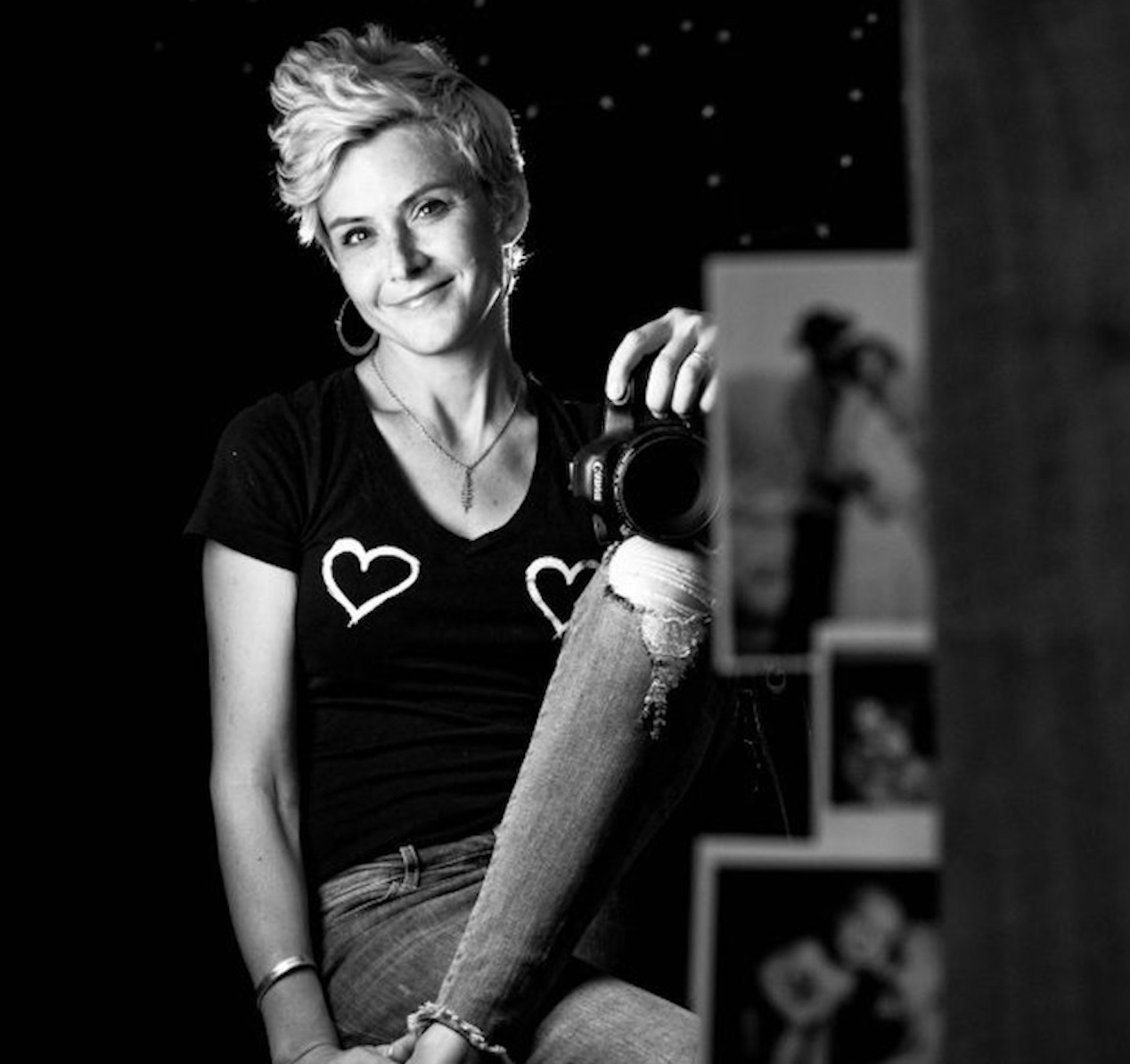
After being diagnosed with breast cancer, photographer, Missy Peters, founded The Breast Cancer Portrait project to encourage women under age 40 to practice breast self-exams.
For High-Risk Women: Mammograms at 30
While there is a wide consensus that women 45 to 54 should have annual mammograms, at age 40, the choice to begin routine mammograms remains between a woman and her doctor, according to guidelines established by the American Cancer Society.
After age 55, women can continue yearly screening, or switch to mammograms every two years — and continue as long as a woman is in good health and expected to live live 10 more years or longer.
“Digital mammography, it turns out, significantly improves the quality of the mammogram,” Dr. Connie Lehman, Chief of the Breast Imaging Division at Massachusetts General Hospital, explains.
Women who fit into the high-risk category for breast cancer — meaning they have a first-degree relative who has had breast cancer, or they have the BRCA1 or BRCA2 gene mutation, or have had radiation to the chest area when you were young – should start mammogram screening as early as age 30, according to Dr. Connie Lehman, Chief of the Breast Imaging Division at Massachusetts General Hospital in Boston and a Professor of Radiology at Harvard Medical School.
What Is ‘Breast Self-Awareness’?
“I'm up against the ACOG (American College of Obstetricians and Gynecologists) who discourage women from performing breast self-exams. In 2017, they published an article stating, "breast self-examination is not recommended in average-risk women because there is a risk of harm from false-positive test results".
RELATED VIDEO: Don't be Afraid to Reach Out to People: Finding an Outlet After Cancer
Instead, ACOG recommended “Breast Self Awareness” which is defined as “a woman's awareness of the normal appearance and feel of her breasts” in a 2017 practice bulletin.
“I encourage women to know their own bodies and to be their own best advocates,” Peters insists. “Touch your boobs, know the terrain, and if something concerns you, don't let a physician tell you "you're too young", "it's just a cyst". The only reliable way to rule out breast cancer is a tissue biopsy.”
Metastatic Breast Cancer At 18
“My doctor said 18-year-olds don’t get breast cancer,” Brittney Beadle told SurvivorNet. Her mastectomy was scheduled for the day of the senior prom. A month later she was told she had metastatic breast cancer: It was “treatable but not curable.”
Breast cancer survivor Brittney Beadle talks about having breast cancer at a young age
Beadle, now 23, has remained determined to live her “best life possible” and in a recent Instagram post added, “we all have this inner power inside us, unlimited, abundant power that we each have access too if we open ourselves up to it. Challenging times, much like cancer can be an opportunity to help us tap into it."
The Breast Self-Exam: Getting It Right
Breast self-examination is an important screening tool, especially when combined with regular physical exams by a doctor, mammography, and in some cases ultrasound and/or MRI. Each of these screening tools works in a different way and has strengths and weaknesses, according to Breastcancer.org which offers these guidelines for self-exams:
Step 1: Begin by looking at your breasts in the mirror.
Stand with shoulders straight and arms on hips, and look for the following:
- Breasts that are their usual size, shape, and color
- Breasts that are evenly shaped without visible distortion or swelling
- If you notice dimpling, puckering, or bulging, bring this to your doctor's attention
- Also check with your doctor if a nipple has inverted or changed position; or you see redness, soreness, a rash, or swelling.
Step 2: Now, raise your arms and look for the same changes
While you're facing the mirror, look for any signs of fluid coming out of one or both nipples (this could be a watery, milky, or yellow fluid or blood).
Step 3: Next, feel your breasts while lying down:
- Use your right hand to feel your left breast; your left hand to feel your right breast. Use a firm, smooth touch with the first few finger pads of your hand, keeping fingers flat and together. Use a circular motion, about the size of a quarter.
- Cover the entire breast from top to bottom, side to side from your collarbone to the top of your abdomen, and from your armpit to your cleavage.
- Follow a pattern to be sure that you cover the whole breast. You can begin at the nipple, moving in larger and larger circles until you reach the outer edge of the breast. You can also move your fingers up and down vertically, in rows, as if you were mowing a lawn. This up-and-down approach seems to work best for most women.
Be sure to feel all the tissue from the front to the back of your breasts: for the skin and tissue just beneath, use light pressure; use medium pressure for tissue in the middle of your breasts; use firm pressure for the deep tissue in the back. When you've reached the deep tissue, you should be able to feel down to your ribcage.
Step 4: Finally, feel your breasts while you are standing or sitting.
Many women find that the easiest way to feel their breasts is when their skin is wet and slippery, so they like to do this step in the shower. Cover your entire breast, using the same hand movements described in step 3.
Lead photo credit: Missy Peters
Learn more about SurvivorNet's rigorous medical review process.


