Navigating the Path Forward: A Guide for Veterans Facing Prostate Cancer
Resources, expertise, and survivor support to help you after a diagnosis
To help you along the way during your fight against prostate cancer, SurvivorNet has developed a series called Navigating the Path Forward: A Guide for Veterans Facing Prostate Cancer.
This series is designed to help you navigate some of the challenges that may pop up during treatment and beyond, from seeking care through the Department of Veterans Affairs (VA) to coping with side effects.

General Information
General information to help along the way
First and foremost, we want to express our deepest gratitude for your service to our country. Your commitment, bravery, and sacrifice have not gone unnoticed.
We understand that receiving a prostate cancer diagnosis is an overwhelming and challenging moment in your life. In the spirit of the military ethos — adapt and overcome — we are here to provide guidance on how to navigate this difficult journey.
To start off, there are a few basic guidelines experts and oncologists often recommend for people facing a recent cancer diagnosis — from taking notes during doctor visits to seeking out second opinions when necessary.
+ Expand and Learn More...
Dr. Heather Yeo, a surgeon at Weill Cornell and an advisor to SurvivorNet, has these tips for patients:
- Have someone come with you to the doctor — It is important to bring a close friend or family member not only to support you, but also to help you understand and digest all the information.
- Take notes — Writing down what you hear can help you focus and create a record of the information so you can refer to it later on.
- Don’t be afraid to get a second opinion — Your doctor won’t be offended if you get a second opinion. It is extremely important to go through the process with a doctor you trust — and make sure you’re getting the best care possible with a doctor you feel comfortable with.
+ Expand and Learn More...
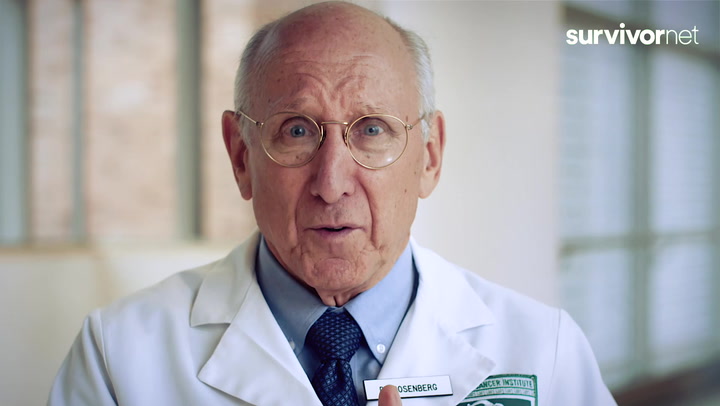
“What would you do if someone in your family got cancer?” We put that question to some of the most renowned cancer doctors in the country. National Cancer Institute Chief of Surgery Dr. Steven Rosenberg recommends seeking out multiple professional opinions to confirm a diagnosis and figure out the options.
Patients should not feel guilty about doing this — as many doctors will recommend and even encourage it.
As we highlight in several areas of SurvivorNet, highly respected doctors sometimes disagree on the right course of treatment, and advances in genetics and immunotherapy are creating new options.
Also, in some instances the specific course of treatment is not clear cut. That’s even more reason why understanding the potential approaches to your disease is crucial.
Just as you relied on your comrades during your military service, now is the time to lean on your support network.
Family members, close friends, fellow veterans, and others can provide emotional support, accompany you to medical appointments, and offer a listening ear when needed. You are not alone in this battle, and your support network is a crucial asset.
Dr. William Breitbart, the chair of the Department of Psychology and Behavioral Sciences at Memorial Sloan Kettering Cancer Center, explained that learning to embrace that uncertainty is a part of living not just for those fighting cancer, but for everyone.
+ Expand and Learn More...
“What the task becomes is having the courage to live in the face of uncertainty, realizing that you cannot necessarily control the uncertainty in life … the suffering that occurs, challenges both good and bad,” Dr. Breitbart said.
“You may not be able to control those but you have control over how you choose to respond.”
Those struggling with feelings of loss of control that cancer can bring can seek help in many different ways — from traditional therapy to support groups for people living with cancer to making lifestyle adjustments to help cope with stress.
Assembling your team
Assembling your treatment team
The process of finding the right doctor and deciding where to get treatment can be stressful in itself. After a diagnosis, establishing clean communication with your team is key.
You should feel comfortable discussing your concerns, asking questions, and actively participating in decisions about your treatment plan.
Regardless of where you are getting treatment, there may be several specialists involved in your care — and you’ll need to work together to find the best treatment approach.
+ Expand and Learn More...
With prostate cancer, your care team may consist of the following specialists:
- Urologist — A surgeon who focuses on treating issues with the urinary tract and the male reproductive system. If you have prostate cancer, the urologist may help with the diagnosis and offer surgery as a potential treatment option. A urologist is often involved in caring for men with prostate cancer through multiple steps in the journey.
- Radiation oncologist — Someone who uses radiation to tackle cancer. Radiation is one of the most used treatments for prostate cancer. Radiation can cure early stage disease and help men live longer who have metastatic disease. A radiation oncologist along with a urologist are most involved in treating prostate cancer in the United States.
- Medical oncologist — A doctor who specializes in using systemic agents like chemotherapy or immunotherapy to treat cancer. They’re trained to diagnose it, figure out how bad it is, and treat it using things like chemotherapy, endocrine therapy, and other medications.
- Physical therapist — A pro at helping people get their strength, mobility, and function back. If you’re dealing with prostate cancer, physical therapy can counter some of the side effects of treatment, like bone weakening from hormone therapy. It can also make you feel more in control of your body and help with stress and anxiety.
- Nutritionist or dietitian — An expert in what your body needs to stay healthy. They can suggest what to eat to keep you strong and combat some of the side effects of treatment.
- Social worker — Can offer counseling and support in many different ways. They’re there when families dealing with prostate cancer face tough challenges.
- Mental health professional — Professionals such as a therapist, counselor, psychologist, or psychiatrist might be helpful to you if you are struggling mentally or emotionally after a diagnosis. Those looking for spiritual guidance may find helpful support from clergy, including hospital chaplains.
- Genetic counselor — A healthcare professional who collects your personal and family health history and uses this information to help determine the likelihood of having a genetic condition or mutation. The genetic counselor can help you decide whether or not genetic testing might be right for you or your family members, and can help explain genetic testing results.
Your Diagnosis
Understanding your diagnosis
During the initial workup for prostate cancer, a tissue biopsy will be obtained. This is typically performed under ultrasound guidance. Various lab tests such as a PSA (prostate specific antigen) and imaging are used to determine if you have localized prostate cancer which is confined to the prostate and surrounding tissues, or metastatic disease, which has spread to distant sites.
+ Expand and Learn More About Prostate Cancer Type...
Prostate cancer imaging has advanced considerably in the last decade. It can provide valuable information regarding the extent of disease with varying degrees of sensitivity. They are typically ordered in patients with an initial diagnosis of intermediate or high risk prostate cancer, recurrent disease, or suspected metastatic disease. they may also be used to track response to treatment in patients with metastatic prostate cancer.
These imaging tests include:
- Multiparametric MRI (mpMRI) of the prostate can be used to identify prostate nodules, extension out of the prostate capsule, and lymph nodes. This may be ordered in patients with suspected prostate cancer to help better target those areas for biopsy.
- Bone scan: Prostate cancer has a high predilection for spreading to the bone. This is a nuclear scan that uses a radioactive isotope, Technetium-99m, to identify areas in the bone where the prostate cancer may have spread. Patients with elevated PSAs, locally advanced disease, or high Gleason scores may have this test ordered.
- CT Scan of the abdomen and pelvis: This is a relatively common scan ordered in patients with intermediate and high risk prostate cancer as well as recurrent disease. It provides a high level of anatomic detail especially in detecting spread to the lymph-nodes, abdominal organs, and bones.
- Positron Emission Tomography (PET) scan: This is another nuclear scan. They may be ordered in the initial staging process, recurrent prostate cancer, and if your doctor suspects you have metastatic prostate cancer. There are a variety of radioisotopes being used in this setting and you may hear terms such as F-18 Fluciclovine (Axumin Scan) or “PSMA-PET.”
Disease course can vary significantly based on several factors, including the initial stage of disease at presentation, an individual’s health, available treatment options, and behavior and genetics of the cancer.
Localized Prostate Cancer
If you present with a more localized disease that has not spread to distant areas, the treatment options may include one or more of the following:
- Radiation Therapy
- Radical Prostatectomy
- Hormone therapy
Because the treatments for localized disease are typically effective on prostate cancer regardless of the underlying genetics, there is often less of a need for genetic testing.
Active Surveillance
It is also important to note that patients with localized prostate cancer deemed low risk have an additional option of active surveillance.
The idea of active surveillance is continued monitoring of the disease with the intention of intervening should the cancer progress. This entails a PSA blood test usually every 6 months along with an annual prostate biopsy or a prostate MRI. Many patients may be spared the side effects of treatment with this approach.
Metastatic Prostate Cancer
Some patients present with metastatic disease on initial diagnosis, and sometimes patients previously treated for localized disease can develop metastatic disease in the years after their initial treatment.
Typically in this setting, systemic treatment with chemotherapy, immunotherapy, and hormone therapy may be used. Radiation may be used in patients that are symptomatic or who have limited areas of spread.
Genetic testing and profiling of the tumor is most often indicated when a patient has prostate cancer that has developed into metastatic disease. The results of this testing have several implications for future treatment. Understanding the testing options and when to get treatment is important when making informed decisions regarding your future cancer care.
The Gleason Score
The Gleason score was devised in the 1960s by Don Gleason, a pathologist at the Minneapolis Veterans Administration (VA) Hospital. He recognized that prostate cancer cells organize themselves into discrete patterns as they change from normal cells to cancer cells. The higher the score, the most aggressive the cancer. The Gleason score is still considered the ultimate indicator of the potential for prostate cancer to grow and spread.
The lowest Gleason score is 6, which is a low-grade cancer. A intermediate-grade cancer is a Gleason score of 7 and a high-grade cancer is a Gleason 8, 9 or 10.
+ Expand and Learn More...
The Gleason score is also critical to determining the stage of your prostate cancer along with local tumor extent, spread to lymph nodes, distant organs, and PSA blood test. It also influences the grade grouping (1-5) of your prostate cancer.
The grading system is not without controversy. For example, doctors often disagree about whether to treat and/or how to treat a low-grade Gleason 6 cancer.
+ Expand and Learn More on The Gleason Score
The Gleason Score determines how aggressive prostate cancer is and also provides information on how to proceed with treatment. To calculate a Gleason grade, the pathologist will study the tumor cells taken from a biopsy and see how the cells are organized. the pathologist then takes the two most common Gleason grades seen under the microscope and adds them together to obtain a Gleason score (i.e. Gleason 3+4=7 for a Gleason 7 prostate cancer).
A Gleason score will let oncologists know when to wait and watch or when to treat, assuming the patient is young enough to benefit from treatment (usually under age 70). Lower numbers translate into better risk factors, and different doctors may approach treatment differently.
Patients who have high-risk cancer, meaning they have high Gleason scores and a high PSA (over 20), will usually be treated aggressively. Studies show that patients who fall somewhere in the middle are likely to benefit from treatment because it prolongs life expectancy. Still, the decision on what approach to choose will depend on several factors, including the risk-benefit ratio of the treatment options.
Molecular Testing
How molecular testing can impact your treatment plan
Next-generation sequencing (NGS), a type of molecular testing, can help you and your doctor decide on the best course for prostate cancer treatment. This sort of testing may be recommended for men with advanced prostate cancer. Genetic or germline testing is also considered very important in both early and advanced stages of prostate cancer.
What are Prostate Cancer Mutations?
DNA damage is an ongoing occurrence that necessitates a sophisticated web of repair mechanisms to uphold the integrity of the genome.
In healthy cells, DNA may sometimes act strangely. When that happens, DNA is repaired via several mechanisms including the homologous recombination repair (HRR) pathway. In the presence of HRR gene mutations (HRRm), cells are unable to effectively repair broken DNA — and that could lead to cancer.
The most famous of these Homologous recombination repair genes are called BRCA1 and BRCA2.
HRR gene mutations occur in approximately 25% of patients with advanced prostate cancer.
+ Expand and Learn More On Hereditary Mutations
Mutations in HRR genes can be hereditary (germline) or sporadic or nonhereditary (somatic).
Around 5% to 15% of prostate cancers come from family traits (hereditary cancer), which means they might run in families. When men have certain special gene changes they inherited, the prostate cancer can be tougher than in those without these gene changes.
If a person’s dad, brother, or son had prostate cancer, his chances of inheriting it become two to three times higher. This chance gets even more likely if more family members had prostate, breast, or ovarian cancers. The age when a close family member got cancer matters, too.
Up to 15% of men with cancer that has spread (metastatic cancer), and 10% of men with cancer that hasn’t spread, have changes in certain genes related to fixing DNA, like BRCA2, BRCA1, ATM, CHEK2, PALB2, and other DNA repair genes (MLH1, MSH2, PMS2, MSH6).
+ Learn More on How Can Molecular Testing Can Impact Treatment...
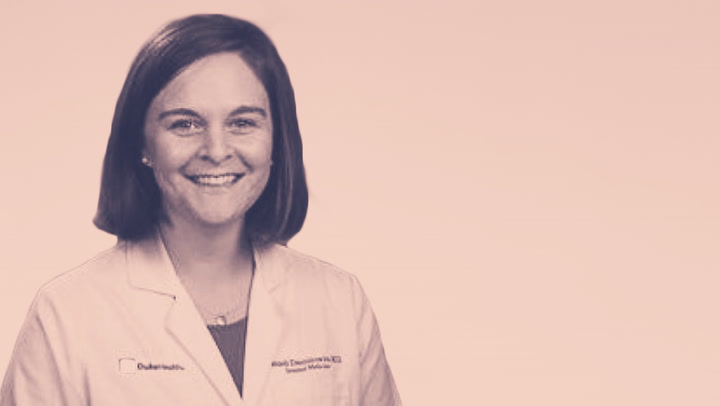
Molecular testing “gives us more tools to personalize that treatment. It gives us more information to understand how a cancer may respond to a treatment. And it gives us more information to make other new treatment options, things like clinical trials or potential options for you, as well,” Dr. Hannah McManus, a genitourinary oncologist at Duke Cancer Center Genitourinary Clinic, told SurvivorNet.
“And I think that’s just going to increase as we do more and more studies and understand how these genetic changes drive prostate cancer. It helps us personalize that treatment and our discussion together even more. So I think it’s really exciting.”
National Comprehensive Cancer Network (NCCN) Guidelines recommend germline and tumor testing for HRRm in all patients with metastatic prostate cancer and consideration of testing for patients with regional disease.
“I think really any patient with prostate cancer can ask their doctor if they should get germline genetic testing or genetic testing, looking to see if they have an inherited mutation that may have made them more at risk for prostate cancer. That can impact your treatment and it can impact your family and potential screening for cancers for them in the future,” Dr. McManus said.
+ Who Benefits From Molecular Testing? Expand and Learn More...
For patients with metastatic prostate cancer (that has spread outside of the prostate), it’s essential that you ask your doctor about genetic testing. These results could guide your treatment plan.
For patients with localized prostate cancer, some of these molecular profiling tests that are available to help guide treatment decisions are used in a little bit more nuanced ways and it is not necessarily right for every patient.
It’s important to have a conversation with your oncologist, who knows all the details of your cancer journey.
“For metastatic prostate cancer, it’s pretty straightforward to me,” Dr. Michael Carducci, a medical oncologist at Johns Hopkins Kimmel Cancer Center, told SurvivorNet.
“I think really every patient with metastatic prostate cancer should be having next-generation sequencing to help guide treatment decisions and making sure all medication therapies are being evaluated. Molecular profiling tests for localized prostate cancer are for very specific situations and there is some controversy around when to use them.”
Treatment
What are my treatment options?
After your treating team has all of the information (PSA, Gleason Score, prostate exam, and the results of any imaging scans), your doctor will use it to categorize your cancer into one of several groups, called risk groups.
These include:
- Low risk
- Intermediate risk
- High risk
There are several subgroups within these categories that your doctor may mention. Which risk group your cancer falls into will determine what treatment options are available to you.
Your treatment may include the following:
- Active surveillance
- Surgery
- Radiation
- Hormone therapy
- Targeted therapy
Your doctor may also recommend a combination of multiple therapies.
When determining the best way to treat cancer, in addition to your risk group, your doctor will also consider other factors, including:
- Your age
- Your overall health
- Your life expectancy
- Your goals for treatment
A combination of all of this information will allow your treating team to discuss all of the options that are available for treating your specific cancer.
The two treatment options offered to patients with non-metastatic prostate cancer are surgery (radical prostatectomy) or radiation therapy. Hormone therapy may be offered depending on the risk group of your prostate cancer.
+ Expand and Learn More About Treatment Options...
Recent prospective data from the ProtecT trial have shown equivalent outcomes in terms of cancer survival and recurrence for radical prostatectomy and radiation therapy. the differences are mainly in their respective side effect profiles.
Radical prostatectomy
This involves removal of the prostate and the formation of a vesico-urethral anastomosis (a connection between the urethra and the bladder). This is usually performed with minimally invasive techniques such as video assisted laparoscopy or with robotic assistance.
A pelvic lymphnode dissection may also be done to sample the lymph nodes if your risk of nodal spread exceeds 2%. The advantage of this approach is that it can offer a definitive cure in a single setting without the need for additional treatment. Patients may also avoid side effects associated with hormone therapy. The most notable side effects of this approach include urinary incontinence and erectile dysfunction. Other side effects include bleeding, infection, urethral stricture, and orgasmic dysfunction.
Radiation therapy
Radiation therapy most commonly uses high energy x-rays to kill prostate cancer cells. There are several modes of radiation delivery. External beam utilizes a linear accelerator to produce x-rays that travel through the body and target the prostate.
Volumetric Modulated Arc Therapy (VMAT) is the most common external beam technique. VMAT alters the intensity of the beam as it rotates around you minimizing the dose to uninvolved organs such as your bladder and rectum. By doing this, it can significantly reduce the risk of developing side effects as a result of radiation treatment.
The advantage of this approach is its non-invasive compared to surgery with equivalent cancer outcomes. The disadvantages are the need for multiple treatments over several weeks and the potential need for hormone therapy should your prostate cancer be deemed unfavorable or high risk.
Side effects may include:
- Fatigue
- Erectile dysfunction
- Urinary urgency
- Diarrhea
- Weak flow of urine
- Burning with urination
Luckily, many of these side effects will resolve in the weeks following completion of radiation.
Brachytherapy is another radiation modality that can be used alone or in combination with external beam. It utilizes a radioisotope which is placed inside the prostate under ultrasound guidance. The advantage of this procedure is it can be completed in a single setting. The disadvantage is it requires extensive pre-operative testing patients are under anesthesia. The side effects include urinary incontinence, urinary retention, proctitis, and erectile dysfunction.
Hormone therapy
Sex hormones such as testosterone are thought to encourage the growth of prostate cancer cells.
Hormone therapy such as leuprolide (Lupron) or relugolix (Orgovyx) can shut down the production of sex hormones. It has been shown to decrease the risk of relapse from prostate cancer as well as improve overall survival.
It is typically indicated in patients with unfavorable intermediate high risk prostate cancers that undergo radiation therapy. It also forms the cornerstone of treatment in patients with metastatic prostate cancer. The duration of therapy ranges from a few months up to 3 years.
The side effects may include:
- Decreased libido
- Hot flashes
- Headache
- Impotence
- Joint aches
- Sweating
The decision as to what treatment approach to consider is highly personal and should be made after discussed the risks and benefits with your doctor.
Living with Cancer
Living with prostate cancer
We understand that a diagnosis of prostate cancer can be overwhelming, and the prospect of surgery and treatment might feel like an arduous journey.
However, it’s crucial to recognize that life after prostate cancer can indeed be fulfilling, and there are ways to navigate this path with hope and optimism.
Surround yourself with a support network of fellow veterans, friends, and family who can provide encouragement and understanding.
As you embark on this journey, remember that your military training has equipped you with the resilience needed to overcome adversity.
You can absolutely have a good sex life after prostate cancer treatment. And, yes, you should feel comfortable talking about it and asking for help.
A large percentage of men suffer from problems in the bedroom, or sexual side effects, as a result of radiation or surgery. Some men may have trouble getting or maintaining an erection, while others can no longer have an erection at all. But there are many ways men can get back to being sexually active, Dr. James Brooks, Chief of Urologic Oncology at Stanford Medicine, explained.
+ Expand and Learn More...
There are several different medications on the market that work for prostate cancer survivors. We’ve all heard of Viagra and Cialis, as well as different devices including the Vacuum Erectile Device (VED). A prosthesis is also an option.
“Prostate cancer can require couples to think more broadly about their intimacy,” Dr. Brooks said. He suggests men talk about with their urologist and perhaps seek counseling with a sex therapist.
Veterans Stories
Inspiring survivor stories
After — or during — the cancer treatment process, it can be really helpful to hear the stories of people who have been through the same struggles and how they coped and learned to live with, and move on from, the disease.
In this section of our Navigating the Path Forward: A Guide for Veterans Facing Prostate Cancer guide, we’re sharing the stories of incredible (and inspiring) prostate cancer survivors.
+ Expand and Learn More on George's Story...
George Crawford, a native New Yorker, has been through a lot in his 81 years. He lived through World War II, he was in the Navy during the Cuban Missile Crisis; he’s done a lot of living and he has a lot of stories to tell. But receiving his prostate cancer diagnosis still came as a big shock.
“When my doctor told me that I had stage four cancer, a very, very aggressive cancer, he didn’t say in so many words I had four months to live … but he gave every signal that he could that this was not a good story at all,” George says. “I told my wife, and I told immediate family, but I asked them not to tell anybody else because I hadn’t even come to terms with it myself.”
Despite his grim prognosis, George happened to get lucky. He was undergoing a summer-long regimen of chemotherapy when his doctor went away to a symposium and was told about a drug called Zytiga — a type of hormonal therapy that blocks the production of androgens, which are the hormones that help prostate cancers to grow. “He came back and he said, there’s a new protocol, you start taking Zytiga as quickly as you can,” George says. “He said I [was] really, basically, the first person in America to do this.”
And the Zytiga worked for George — over time, his prognosis got better and batter. And after all was said and done, George says something good did come out of his cancer journey — it brought his family closer together.
+ Expand to Learn More About Mike Crosby's History
For as long as he can remember, Mike Crosby wanted to fly.
When he got prostate cancer, his wife explains, “I knew he would land this, just like he landed everything else.”
Crosby is now 63-years-old. He’s a retired Naval Commander whose call sign was “Bing.” He beat prostate cancer three times and has now turned his diagnosis into a new life of service by offering much-needed hope and resources to veterans also dealing with the disease.
“We’re not taking care of these guys, and we need to do a better job,” Crosby, 63, told SurvivorNet from his home in San Diego.
More Resources
Living with Prostate Cancer
We have made it to the end of the Navigating the Path Forward: A Guide for Veterans Facing Prostate Cancer series. We hope that you were able to find some helpful information and some of the support you are looking for as you embark on your journey as a cancer survivor.
Remember that life after prostate cancer can be a new chapter filled with hope, renewed purpose, and meaningful experiences.
Be sure to check out SurvivorNet’s designated Prostate Cancer section for a breakdown of the basics of the disease, treatment options, and what you can expect as a survivor.
Embrace the support available to you, and don’t hesitate to seek guidance from fellow veterans who have navigated similar paths. Your journey may be challenging, but with the strength that defines you as a veteran, there is immense potential for a fulfilling life beyond prostate cancer.
At SurvivorNet, we’re here to help survivors navigate the complex world of living with cancer. Thank you for being part of the family!