Using Cannabis to Help Manage Multiple Sclerosis Symptoms
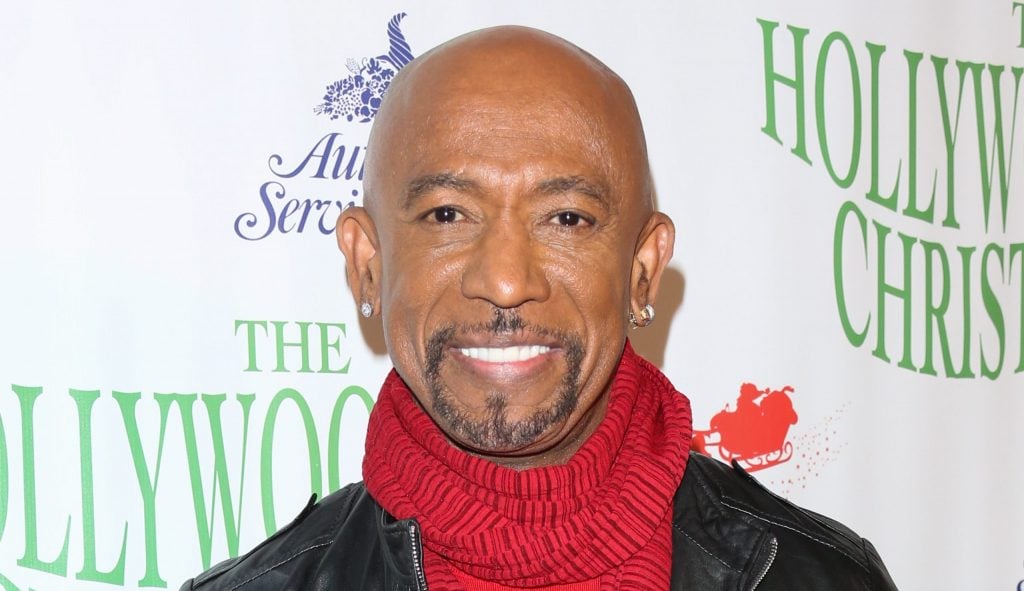
- Former talk show host Montel Williams, 69, credits medical cannabis as a “lifeline” in managing chronic pain and improving his quality of life while living with multiple sclerosis.
- Multiple sclerosis affects the brain and central nervous system, causing symptoms like fatigue, numbness, and coordination issues; while incurable, therapies and assistive tools can improve daily function.
- Research published in peer-reviewed journals, including the International Journal of MS Care, supports cannabis use for MS symptom relief, with studies showing improvements in pain (72%), spasticity (48%), and sleep (40%)—especially through oromucosal sprays and oral forms. Talking with your doctor is recommended before exploring cannabis as an option.
- Although MS does not have a cure, common tools such as wheelchairs, canes, leg braces, and some medical treatments called disease-modifying therapies (DMTs) may improve the quality of life for people living with the disease.
- A study in American Family Physician found that DMTs “have been shown to slow disease progression and disability; options include injectable agents, infusions, and oral medications targeting different sites in the inflammatory pathway.”
“It’s been a lifeline for me,” William said in an Instagram post.
Read MoreAdditional published research released in December 2022 in the peer-reviewed “International Journal of MS Care” found that within its own study involving 141 patients with multiple sclerosis, “Patients experienced extensive MS symptom improvement after initiation of MC, with alleviation of pain (72% of patients) and spasticity (48% of patients) and improvement in sleep (40% of patients) the most common.”
View this post on Instagram
Multiple sclerosis is a disease of the brain and central nervous system that causes numbness or tingling in the limbs, fatigue, lack of coordination, blurry vision, and unsteady gait.
Although MS does not have a cure, common tools such as wheelchairs, canes, leg braces, and some medical treatments called disease-modifying therapies (DMTs) may improve the quality of life for people living with the disease.
It should be noted that administering cannabinoids orally and smoking them are not quite the same, as smoking comes with risks.
Using cannabis for medical reasons can come with some uneasiness, especially since it still carries a negative stigma, and it is still illegal in some cases. However, medical marijuana use is legal across most of the country.

According to the Centers for Disease Control and Prevention (CDC), “As of February 2024, 47 states, the District of Columbia, and three territories (Guam, Puerto Rico, U.S. Virgin Islands) allow for the use of cannabis for medical purposes.”
Williams says that stigma still keeps some patients from accessing the care they need, whereas cannabis can be helpful. He hopes that by talking about it more openly, he can help lessen that stigma’s influence.
Helping Multiple Sclerosis Patients with Resources
Why You Should Tell Your Doctor If You Use Cannabis
Although some experts disagree with cannabis use, SurvivorNet understands it is legal in parts of the country, and there are some medicinal uses for it. If you are using cannabis, Dr. Brian Berman, professor of family community medicine at the University of Maryland School of Medicine, says users should tell their doctor about their cannabis use, especially if it is consumed through smoking.
“I think that you should always tell whichever therapy we’re talking about, you should always inform your oncologist and your physician, this is (using cannabis) what you’re doing,” Dr. Berman tells SurvivorNet.
Each state has its own requirements for obtaining a medical marijuana card. If you live in a state where medical marijuana use is legal and you think it might be the right treatment for you, start by talking to your doctor.
“Medical cannabis, if you think about it, is the only botanical medicine that can help nausea, increase appetite, decrease pain, and elevate mood,” Dr. Junella Chin, an integrative cannabis physician in New York, tells SurvivorNet.
Dr. Chin says she often sees patients seeking relief from the side effects of chemotherapy, which may include nausea, pain, decreased appetite, and depression. She says some physicians prescribe Marinol, or synthetic cannabis, to treat these side effects. However, she believes using the actual cannabis plant is much more helpful when used to relieve symptoms.
The cancer risks associated with smoking cigarettes are well documented. However, some experts believe with conviction that cancer risks extend to smoking cannabis as well. Dr. Raja Flores, who is the Chairman of the Department of Thoracic Surgery for Mount Sinai Health System, is among those who believe cannabis fuels cancer risks. “Smoking marijuana likely causes lung cancer independent of cigarette smoking status,” Dr. Flores told SurvivorNet.
“I do think for cigarettes, there is a genetic predisposition to get lung cancer. As well as a genetic predisposition for substance abuse. So, it would not surprise me that there is a genetic link to lung cancer from smoking weed,” Dr. Flores continued.
“As someone on the front lines, who sees this every day, I’ve seen lung cancer caused by marijuana that is incredibly aggressive,” Dr. Flores previously told SurvivorNet.
“There is no really good population-based study that looks at marijuana smoking, and that has had enough time elapsed to show it’s associated with lung cancer, [but] I’ve seen it. I’ve seen multiple cases of it. I see it every day,” he added.
Montel Williams’ Multiple Sclerosis Journey
In a revealing conversation on the “Frankly Seniors” podcast, Williams, 68, described how his symptoms began surfacing as early as 1979 while he was serving in the military at peak physical condition.
“Throughout my entire military career, every three to four months, I went to the doctor, trying to figure out what was going on with my shoulder, back, leg, and hips,” he recalled.

Despite experiencing recurring issues like tingling, pain, and visual disturbances, Williams said he was repeatedly dismissed. At the time, MS was widely believed to affect mainly white women of northern European descent—an image that didn’t match his own.
“Back then, in the physician’s desk reference, when they looked up MS, it said a disease that mostly affected women of northern European descent,” Williams said. “So, here I am, an African-American male getting ready to graduate from the Naval Academy, and I was probably in the shape of my life, and I’m demonstrating so many symptoms that nobody can explain.”
Williams attributes his diagnosis in part to his maternal ancestry. “Part of the reason for that is my family lineage. My mother happens to be half Caucasian, and her mother was from Scotland, and her father was African-American. Through her, that gene came through, skipped a generation, and hit me.”
Over the years, Williams says doctors often pointed to other potential causes, including his past time as a competitive bodybuilder. He remembers one physician advising him, “Quit putting all of that weight on your back, and you’ll feel better.”
Eventually, after nearly two decades of unexplained symptoms, Williams was formally diagnosed with multiple sclerosis—a chronic illness that affects the brain and central nervous system. He described his condition as largely stable today but acknowledged that it remains a constant presence in his life.
View this post on Instagram
“Luckily, I have not had a bout in the last four to five years, and my disease has been very stable,” he said. “However, I still have symptoms that I deal with on a daily basis. However, I’m one of those people who can say that I have MS, but MS is never going to have me.”
Williams’s candid reflections not only highlight the challenges of diagnosing MS in underrepresented communities but also underscore his resilience—a trait that continues to define his life both on and off the public stage.
Learn more about SurvivorNet's rigorous medical review process.

