How a WWII Vet Finds Hope In Immunotherapy Cancer Treatment
- A 102-year-old World War II veteran and grandfather was diagnosed with stage 3 melanoma—a serious form of skin cancer known for its ability to spread—after discovering a lesion on his leg.
- Melanoma begins in melanocytes, the cells responsible for producing pigment in the skin, hair, and eyes. When these cells mutate, they can spread to other parts of the body.
- The WWII veteran is now undergoing treatment with Keytruda, an immunotherapy drug that helps the immune system recognize and attack cancer cells.
- Unlike traditional treatments that target cancer directly, immunotherapy boosts the body’s natural defenses, often resulting in fewer side effects and less damage to healthy tissue.
- Early detection is key: watch for new skin spots or changes in existing moles—especially shifts in size, shape, or color—as these can be early signs of melanoma.
Fay first noticed a suspicious spot on his leg, which turned out to be an advanced form of skin cancer – melanoma – known for its ability to spread rapidly. Despite the seriousness of the diagnosis, his condition has remained stable.
Read More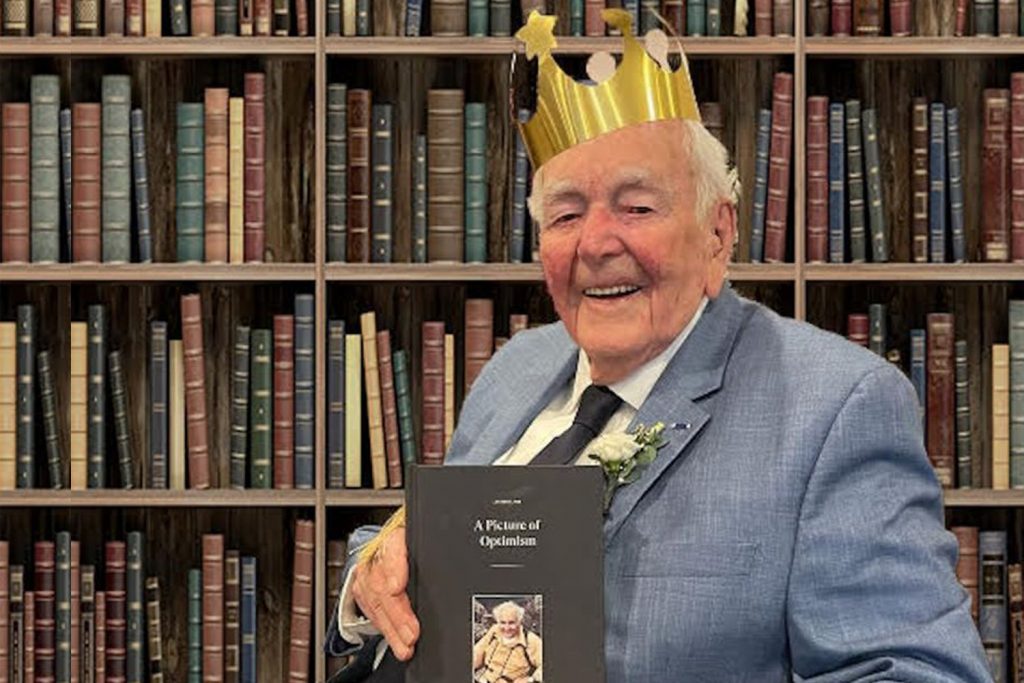
“It was very hard to take in and accept [his] diagnosis so soon after losing my wife,” Fay shared, reflecting on the emotional toll of facing cancer while grieving.

Melanoma begins in melanocytes—the cells that give color to our skin, hair, and eyes. When these cells mutate, they can become aggressive and spread to other organs. While melanoma most often appears on sun-exposed areas like the face, neck, arms, and legs, it can also develop in less obvious places such as the palms, soles, eyes, mouth, or under the nails.
Finding Hope in Immunotherapy
Fay’s family turned to immunotherapy—a treatment that empowers the body’s own immune system to recognize and attack cancer cells. For someone of Fay’s age, it offered a less invasive alternative to traditional treatments like chemotherapy or surgery.
“We had heard of immunotherapy in vague terms, but didn’t fully understand how it was being used in melanoma. At the age of 98, it seemed like the least intrusive approach to take for my father,” Paul said.
“Fortunately, he hasn’t experienced any of the side effects, which, honestly, were not that alarming considering the alternative.”
Now, four years after his diagnosis, Patrick Fay continues to defy the odds—living proof that courage, family, and modern medicine can make a powerful team.
WATCH: How Immunotherapy Works
That’s where immunotherapy comes in. These drugs are designed to block the cancer’s protective signals, allowing white blood cells to properly recognize and attack the cancer cells. Interestingly, cancer cells themselves aren’t always hard to destroy, but they multiply rapidly. Immunotherapy helps the immune system keep the cancer in check before it can spread further. It’s essential to remember that immunotherapy may not be effective for everyone.
Fay’s immunotherapy treatment is called Keytruda.
Mr. Fay still undergoes regular check-ups, including PET scans, to monitor the cancer amid ongoing treatment.
How Immunotherapy Like Keytruda Works
Cancer cells often fly under the immune system’s radar by producing proteins that disguise them as “normal.” Checkpoint inhibitors such as Keytruda break that illusion, helping white blood cells recognize and attack those cancer cells.
Rather than killing cancer directly, these treatments empower the immune system to do the job, with fewer side effects on healthy tissue.
WATCH: Immunotherapy Helps Your Body Help Itself
Common side effects of Keytruda include:
- Fatigue
- Rash or itching
- Shortness of breath or cough
- Nausea, vomiting, or appetite loss
- Diarrhea or constipation
- Low thyroid levels
- Abdominal pain
RELATED: Some Melanoma Survivors See Long-Term Side Effects After Immunotherapy Treatment, According to Study
Understanding Melanomas
Melanoma starts in the same cells that give your skin, hair, and eyes their color. In melanoma, the cells change in a way that allows them to spread to other organs.
Changes to a mole you’ve had for a while or a new growth on your skin could be signs of melanoma, according to SurvivorNet’s experts. You’ll want to watch them and tell your doctor about any changes you notice.
WATCH: How do you perform a skin check using the ABCDEs?
SurvivorNet experts recommend avoiding unprotected sun exposure because ultraviolet (UV) radiation can lead to melanoma. Tanning beds pose ultraviolet radiation risks for skin cancer and should be avoided. Many dermatologists recommend using spray tans to reduce the risk of melanoma skin cancer.
The most important thing to look out for when it comes to finding melanoma is a new spot on your skin or a spot that is changing in size, shape, or color, SurvivorNet’s medical experts say.
Treatment options for melanoma include targeted therapy and immunotherapy, which give people a better chance of living a long and healthy life than ever before. If you’re diagnosed with melanoma, there’s a good chance surgery will be the treatment your doctor recommends. Cancer removal usually leads to a cure in the early stages of the disease. After surgery, the removed tissue and lymph nodes are examined to measure the melanoma and determine if it has clear margins. Clear margins mean the cells around the area of tissue that was removed don’t contain any melanoma. When no cancer cells are left around the removed area, your cancer is less likely to return.
WATCH: Beating Aggressive Melanoma: An Immunotherapy Success Story
For melanoma patients who need additional treatment after surgery, they are likely to receive adjuvant therapy (treatments administered after surgery). Adjuvant therapy is designed to improve outcomes and decrease the risk of recurrence.
Questions to Ask Your Doctor
If you are diagnosed with skin cancer, you may have some questions for your doctor. SurvivorNet suggests some of the following to help you on your cancer journey.
- What type of skin cancer do I have?
- What treatment options exist for my type of melanoma?
- Will insurance cover this treatment?
- Would treatment through a clinical trial make sense for me?
- What resources exist to help manage my anxiety because of this diagnosis?
Learn more about SurvivorNet's rigorous medical review process.

