Focusing on Positivity While Facing Cancer
- As “General Hospital” star John York is battling two blood and bone marrow disorders, myelodysplastic syndromes (MDS) and multiple smoldering myeloma, we’re admiring his optimistic outlook on life.
- Aside from fighting cancer, the Illinois-born TV star is hoping to save at least one life by spreading awareness and inspiring people to sign up to be an organ donor on BeTheMatch.org.
- MDS is a variety of bone marrow disorders that look similar: under a microscope, the bone marrow cells look like cancer, and genetically may have alterations that are known to cause MDS, SurvivorNet’s experts explain.
- “You can think of MDS as a spectrum of diseases,” Dr. Lewis Silverman, director of the resource center for MDS at Mt. Sinai’s Tisch Cancer Institute, told SurvivorNet in an earlier interview. “On the one hand, there are patients who, when they present, are categorized as having very low-risk disease, and then it ranges up through middle categories to very high-risk disease. MDS patients can be categorized anywhere along that spectrum of disease.”
- Smoldering multiple myeloma is a disease that is very close to becoming active myeloma, but does not have any symptoms.
- Experts also tell SurvivorNet that maintaining a positive attitude and continuing to do things that make you happy, like York has, can have a real impact on treatment outcomes and how a patient feels overall.
The 64-year-old actor recently went public about the rare type of blood cancer he’s been diagnosed with, revealing he’s stepping away from work to focus on his health.
Read More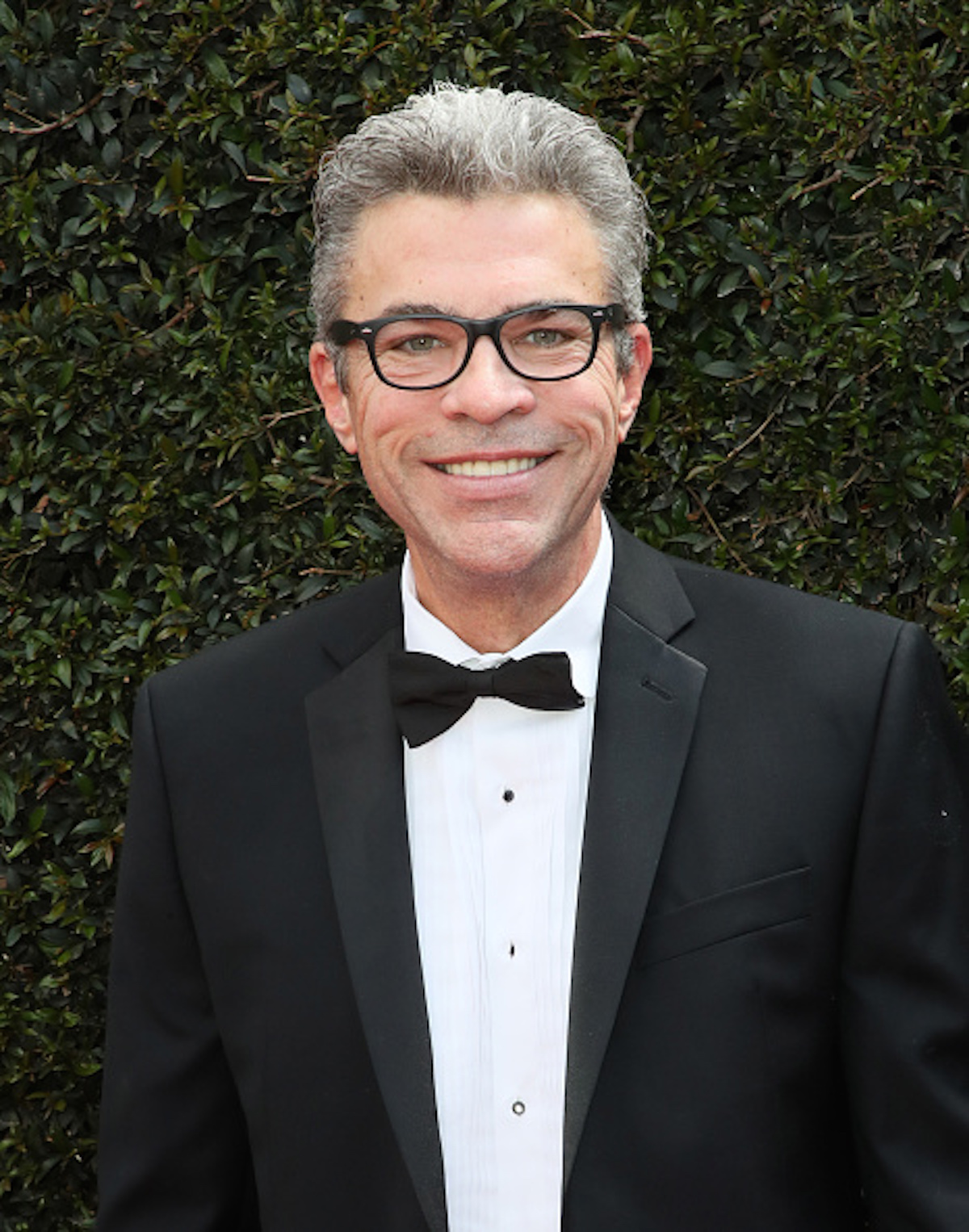
“I went through life with colonoscopies, medicines, the whole thing, and always had to be under doctor’s care,” he explained, insisting he’s always optimistic, “living life” and feeling as if “everything’s good.”
Recounting how felt after learning he had cancer, York said, “I mean, I walk three miles a day and I’m in great shape. And my diet is great and my appetite is great.”
His doctor credited the reasoning behind his body feeling like nothing was wrong, due to catching the cancer “early.”
As for his outlook on the treatment he’s undergoing, he told the news outlet, “It is what it’s, you know what I mean?
“And then everybody’s gotta get their treatment. And then you go home, go about your life and you play with the kids. And here we are.”
Expert Coping Resources
- SN & You Presents Mental Health: Coping With Emotions
- Do You Have a Question About Mental Health & Cancer– Strong In Cancer — A New Column From SurvivorNet with Dr. Marianna Strongin
- Resilience: Staying Positive Despite Adversity
- 7 Cancer Survivors Share How Gratitude, Faith, & Seeking the Good In Life Help Give Them Strength
- 7 Tips for Cancer Survivors to Have the Energy You Need
As he remains in search of a bone marrow donor and is now on a donor priority list he’s hopeful for the future and “excited.”
“Many of my family members tested. I believe that the age range is like 18 to 40 to join the registry at bethematch.org/matchformac,” he added, saying that if he can save just one life “that’s huge.”
York further opened up on how he views his cancer journey, telling PEOPLE, “My whole philosophy is one day at a time; whatever they need me to do. Well, if I’m staying in a hospital, I’ll stay in a hospital. If I can go home, I’ll go home, where we have a place where I can be by myself, you know, away from the kids.”
“It goes without saying that Vicki [his wife] is taking on the caretaker role. She’s that now, and she’s been that way forever,” he explained, calling his wife the “the guiding force.”
York is married to his wife Vickie Manners, whom he shares a daughter with.
Despite his wife having fear amid his caner journey, York insists he’s feeling “great,” concluding, “Personally, I feel like it’s in God’s hands. God’s will be done. It’s gonna work out okay, one way or another. I’m either gonna survive or I’m not. And life goes on and things are gonna be okay for everybody… Let’s just go one day at a time.”
John York’s Cancer Reveal
John York took to X, a social media platform formerly known as Twitter, to inform the public about his cancer battle, telling his fans,” Well, hey, you guys, how you doing? It’s me. I said I was going to give you an update on the reason I’m taking a little hiatus from General Hospital, and here it is.
“So, last December of 2022, I was diagnosed with myelodysplastic syndrome or MDS and multiple smoldering myeloma, two blood and bone marrow disorders.”
He continued, “Over the past many months, I’ve had three bone marrow biopsies. Many chemo treatments. I have another one coming up in a couple of weeks. And I’m closing in on a blood stem cell transplant.”
Hey gang, here’s the update, Check out @bethematch if you want to support https://t.co/AxA8xTbDcq pic.twitter.com/ZBinOwIrpd
— John J York (@JohnJYork) September 13, 2023
“Ive been working with some wonderful people at Be The Match to find a potential donor on their registry,” he added. “If it’s possible and you would consider being a donor, joining their registry, for not just me but thousands and thousands of other people who are in need of a donor, go to bethematch.org/matchformac.”
He said his “break” from work will last approximately three to four months. However, he insists he’ll return soon and will keep everyone updated along the way.
Understanding Myelodysplastic Syndrome (MDS)
White blood cells, red blood cells, and platelets develop from specialized stem cells in your bone marrow, the spongy tissue inside some of your bones, such as your hip and thighbone.
Because these specialized stem cells are the blueprint for your blood cells over your entire lifespan, any error that occurs either through normal aging or due to certain stressors (such as prior chemotherapy or radiation) can lead to abnormal development and/or function of the stem cells. Accumulation of these errors can cause cancer.
Acute leukemia is the most aggressive type of blood cancer, but there are several other blood cancers that can develop into an acute leukemia. The most common cancer that can evolve into acute myelogenous leukemia (AML) is called myelodysplastic syndrome (MDS).
Dr. Jun Choi, a Hematologist/Oncologist at NYU Langone’s Perlmutter Cancer Center, Explains MDS
Dr. Jun Choi, a hematologist/oncologist at NYU Langone’s Perlmutter Cancer Center, previously spoke with SurvivorNet about MDS, saying, “When there is a dysfunction in the bone marrow, there is a production of defective blood cells, and there is also a deep decrease in the production of blood cells.
“So the consequence of that is low blood cells in your bloodstream…MDS affects all types of blood cells and ultimately it is a considered a bone marrow failure disorder.”
RELATED: How Does A Bone Marrow Transplant Treat MDS?
MDS is a variety of bone marrow disorders that look similar: under a microscope, the bone marrow cells look like cancer, and genetically may have alterations that are known to cause MDS. Symptoms of MDS include frequent infections, fatigue or shortness of breath (anemia), or easy bleeding/bruising. These symptoms are the result of the bone marrow not being able to produce enough healthy, functional blood cells, SurvivorNet experts explain.
Because some patients with MDS will have their cancer evolve into AML, it is important for your doctor to monitor risk. There are several ways to do do this, but doctors will look at:
- A patient’s blood counts
- The amount of cancer in the bone marrow
- The presence of certain genetic abnormalities on the cancer cells
“For the workup of MDS, you start with a regular blood check and you confirm that someone has low blood cells,” Dr. Choi explains. “And then when the suspicion for MDS is high, the ultimate gold standard diagnostic test is a bone marrow biopsy. And that is because the bone marrow is where all the blood cells are made. And we want to confirm that there is abnormal cells in the bone marrow.”
A bone marrow biopsy can confirm MDS. It can also provide other details on your cancer.
“The biopsy has to be reviewed by the pathologist to see if there is what’s called dysplasia in the blood cells. Dysplasia is abnormal-looking young blood cells that we also want to send the bone marrow sample to assess for any genetic changes,” Dr. Choi says.
“And whether there is any abnormal changes in your chromosome, in the blood cells inside the bone marrow. And based on those, we can categorize the MDS into different categories, different types, and ultimately they can also help us guide the treatments and the prognosis as well.”
Learning About Smoldering Multiple Myeloma
Smoldering multiple myeloma is a disease that is very close to becoming active myeloma, but does not have any symptoms.
“Just by its name, it’s smoldering, it’s almost there to light up the fire, to become active disease,” Dr. Irene Ghobrial, myeloma specialist from the Dana Farber Cancer Institute, previously told SurvivorNet.
Almost all patients diagnosed with active multiple myeloma had smoldering myeloma previously, but most don’t know it. Smoldering myeloma is symptomless, but is characterized by higher levels of abnormal proteins in the blood and plasma cells that make up greater than 10% of the bone marrow.
The chance of progressing to malignant myeloma differs based on the riskiness of the smoldering myeloma. Patients with smoldering myeloma typically have a 10% lifetime chance of progressing to active multiple myeloma, but patients with high risk smoldering myeloma have a 50% chance of progressing to active multiple myeloma within just two years following diagnosis.
RELATED: How to Diagnose and Treat Smoldering Multiple Myeloma
Doctors are making advances on how to diagnose and treat smoldering myeloma. There are two ways high risk smoldering multiple myeloma is diagnosed. First, the bone marrow is measured to see if it is made up of 10% or greater plasma cells. Second, the blood is measured for the presence of certain antibodies. Patients with these results in diagnostic tests should meet with their physicians to discuss potential early treatment options.
So once the diagnosis is made, how is high risk smoldering myeloma treated? The current approach is to “watch and wait.” However, waiting too long can produce active myeloma and serious symptoms. The changes in the blood and bone can eventually become worse, and end up affecting different parts of the body, producing symptoms like bone fractures and organ damage.
Once these injuries occur, patients are started on a three-phase myeloma treatment, which includes steroids, immune system-activating drugs, chemotherapy, and stem-cell transplantation.
Researchers like Dr. Ghobrial, however, are working to develop treatments that can potentially cure patients of the disease before they develop serious symptoms or active myeloma.
“We’ve done several clinical trials, by giving them an immune antibody that activates the immune system, and by killing the cells early, potentially we have a better response to therapy than when we wait for them to have too much disease burden [and] too many changes [to] immune suppression.”
Categorizing Myelodysplastic Syndrome (MDS)
Determining treatment will depend on several factors, as your doctor will assess blood counts, bone marrow, the number of immature cells in marrow, and how cells mature.
“You can think of MDS as a spectrum of diseases,” Dr. Lewis Silverman, director of the resource center for MDS at Mt. Sinai’s Tisch Cancer Institute, told SurvivorNet in an earlier interview. “On the one hand, there are patients who, when they present, are categorized as having very low-risk disease, and then it ranges up through middle categories to very high-risk disease. MDS patients can be categorized anywhere along that spectrum of disease.”
For low risk MDS, no treatment may be necessary, but many patients will need medications or blood transfusions to help improve their blood counts. (A blood transfusion is a procedure in which donated blood or blood components are given to you through an intravenous line.)
For high risk MDS, more aggressive therapy is needed most commonly this will be a “hypomethylating agent” (HMA). These medications work by disrupting unregulated cancer cell growth. A stem cell transplant can also be considered, which is potentially curative. Hematopoietic stem-cell transplantation (HSCT) is a medical procedure that consists of infusing healthy stem cells (from a matched related or unrelated donor) after a short course of chemotherapy or radiotherapy, or both.
While stem cell transplants can be potentially curative, they are not an option for all patients.
“The treatments that we have right now still are not curative except for stem cell transplants, and those are major undertakings, and not every individual is a great candidate for that,” Dr. Silverman explains. “We do evaluate the patients for stem cell transplants and transplant those [eligible] patients.”
Factors such as the patient’s age and overall health need to be considered when determining if a stem cell transplant should be done.
Learning About MDS Treatment
MDS is treated based on symptoms and the risk for it to evolve into AML. Doctors gather information about circulating blood counts, bone marrow findings, and the presence of genetic mutations to determine risk.
Dr. Eytan Stein, Chief of the Leukemia Service at Memorial Sloan Kettering Cancer Center, Explains How Doctors Determine When/How To Treat MDS
For lower-risk MDS:
- Many people may only need to monitor blood counts every few months without needing specific treatment.
- Some people may be started on medications to stimulate RBC or platelet production.
- Some people may need a blood transfusion every few months.
- Specific types of MDS may benefit from lenalidomide (Revlimid), luspatercept (Reblozyl), or immunosuppressing medications.
For higher-risk MDS:
- Treatment usually starts with a class of drugs known as hypomethylating agents (HMAs). HMAs include intravenous or oral forms of azacitidine (Vidayza, Onureg) or decitabine (Dacogen, Inqovi).
- Other treatments are possible depending on the presence of certain mutations or if the disease is more aggressive.
- Some patients may require more frequent transfusions, from every few weeks to even several times a week.
- Some patients may be eligible for a bone marrow transplant.
- Many patients should consider enrolling in a clinical trial if available.
Because the diagnosis, prognosis, and treatment plans offered depend on appropriate testing, it is important to talk to your doctor about whether molecular testing on your bone marrow biopsy has been conducted. This may also provide opportunities for clinical trials in the future.
RELATED: ‘I Want to Thrive’: Breast Cancer and MDS Survivor Rob Roberts Gives Post-Treatment Update
Additionally, we recommend asking your doctor if referring for a bone marrow transplant is right for you. Although MDS generally affects older adults, there is no “age limit” for doctors to consider a potentially curative transplant, as long as you are otherwise healthy.
Dr. Choi explains that the treatment approach for MDS depends on several factors:
- The type of MDS
- The prognostic score
- A person’s age & overall health
“The only curative option [for] MDS these days is a bone marrow transplant,” Dr. Choi explains. “Now, bone marrow transplant is one of the more intense therapies for MDS, so you really want to be able to tolerate this therapy. That is why this therapy is reserved mostly for younger patients and [those] who do not have other medical conditions.”
However, the majority of patients diagnosed with MDS are older, so a stem cell transplant may not be an option. While the disease may not be cured, it can be managed.
“One of the goals for patients with higher risk disease is to extend survival and manage symptoms,” Dr. Silverman explains. “One of the treatments that we utilize are drugs called hypomethylating agents (HMAs). These drugs convert disease from an acute type of disease … the drugs are able to convert disease into a more chronic type of disease, which patients can live with while they’re getting treatment.”
RELATED: Stem Cell Transplants – Understanding the Risks
Dr. Silverman added that patients are often able to go along with their daily lives, aside from the time spent getting treatments.
Drugs such as azacitidine (Vidaza) or decitabine (Dacogen) may be suggested for people whose MDS is considered lower risk. These drugs have the potential to improve blood counts, quality of life, and could help people live longer.
There are different approaches for people who have different types of the disease. For example, if a person has the del(5q) type of MDS, a drug called lenalidomide (Revlimid) may be used.
MDS may be treated with the following approaches:
- Disease modifying therapies, such as chemotherapy or targeted therapy
- Supportive care, which could include blood transfusions or blood-stimulating medicines
- Bone marrow transplants
- A combination of the above approaches
There is also the option to participate in clinical trials, which test out new drugs that are in the experimental phase and have not yet received FDA approval.
For patients seeking new approaches to treating MDS, and those who have not responded to treatments, clinical trials may be an option.
RELATED: Check out SurvivorNet’s Clinical Trial Finder
“So many universities, such as our own institution — NYU Langone — offer many clinical trials to target particular cancers,” Dr. Choi explains.
“In my specialty, we have many different trials to treat patients with difficultly, treat patients with leukemias and MDS — and we have options for those who have never [undergone] any treatments all the way to someone who has seen a number of treatments … These options are ideal for someone who wants to really look for a new drug that has yet to be proven, but seems to be pretty promising in the future.”a
Focusing on the Positive Amid Cancer
John York’s admirable positive attitude even while battling incurable stage 4 cancer is inspiration. His resilience and bravery to keep focusing on things that bring him joy and smiles to the faces of his loved ones is certainly remarkable quality.
This is something Dr. Zuri Murrell, of Cedars-Sinai says helps a cancer patient’s prognosis.
“A positive attitude is really important,” Dr. Murrell previously told SurvivorNet.
“My patients who thrive, even with stage 4 cancer, from the time that they, about a month after they’re diagnosed, I kind of am pretty good at seeing who is going to be OK. Now doesn’t that mean I’m good at saying that the cancer won’t grow,” Dr. Murrell says.
WATCH: Dr. Zuri Murrell discusses the power of positivity.
Other experts SurvivorNet have spoken to recommend that anyone facing cancer make sure they continue to prioritize their overall well-being and do the things that they love, just like York is doing.
Dr. Dana Chase, a gynecological oncologist at Arizona Center for Cancer Care, says people with cancer should be making time to do things that make them happy.
“We know from good studies that emotional health is associated with survival, meaning better quality of life is associated with better outcomes,” Chase said.
Dr. Dana Chase discusses the importance of patients finding joy during treatment.
“So working on your emotional health, your physical well-being, your social environment [and] your emotional well-being are important and can impact your survival. If that’s related to what activities you do that bring you joy, then you should try to do more of those activities,” Dr. Chase explained.
Questions to Ask Your Doctor
If you’re battling cancer or on the other side of it, and you’re struggling with your outlook on life, here are some questions you may consider asking your doctor to get the conversation started:
- What can I do if I’m struggling to be thankful for what I have in my life?
- Are there local resources for people wishing to improve their mental health?
- What else can I do to help reduce my stress level during my cancer journey?
- It’s difficult for me to find happiness and joy. How can I find help?
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

