The Importance of Breast Cancer Screenings
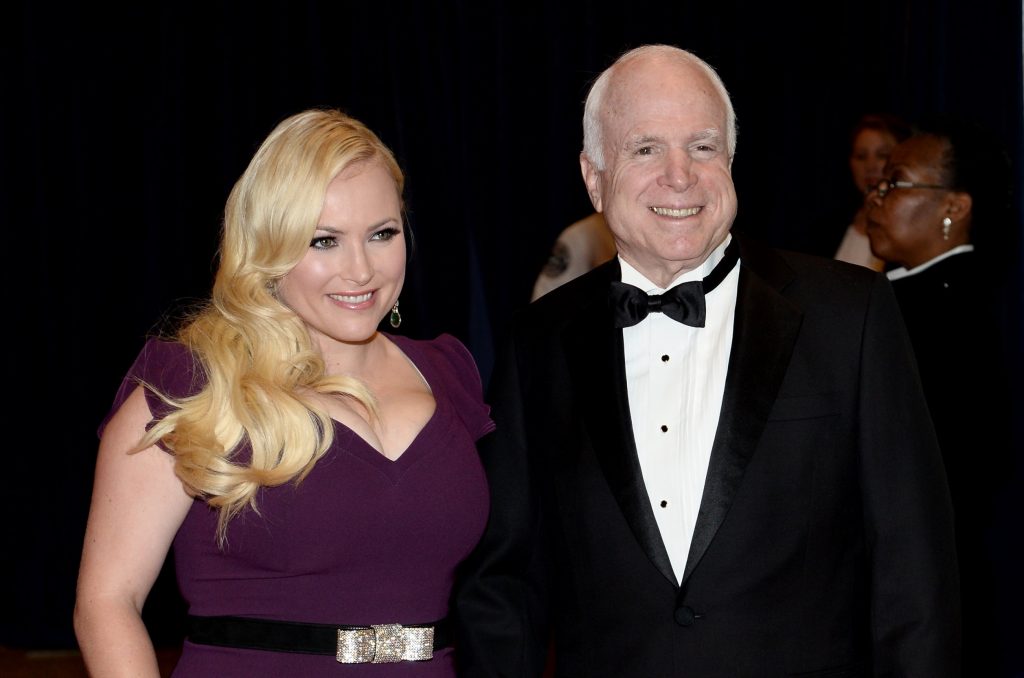
- Meghan McCain, who lost her dad the late John McCain, to an aggressive type of brain cancer in 2018, is spreading awareness on the important of breast cancer screenings after a recent biopsy of a mass on her breast was declared benign.
- The U.S. Preventive Services Task Force recommends women with average breast cancer risk begin screening mammograms once every two years at the age of 40.
- It’s important to note that women with the BRCA gene mutation, who have a family history of cancer, or have dense breasts are at higher risk and should talk with their doctor about when to begin screening. It may be younger than 40.
- For women aged 55 and older, the American Cancer Society recommends getting a mammogram every other year. However, women in this age group who want added reassurance can still get annual mammograms.
- Women with dense breasts are at a higher risk for developing breast cancer because dense breast tissue can hide potential cancer during screening. 3D mammograms, breast ultrasound, breast MRI, and molecular breast imaging are options for women with dense breasts for a more precise screening. It is important to ask your doctor about your breast density and cancer risk.
- Studies have shown that people who practice gratitude, consciously taking stock of the good things in their lives, report more happiness and less stress. Anecdotally, doctors say that patients who live with gratitude and a positive attitude, like McCain, tend to respond to treatment better, even in difficult situations.
McCain, a 40-year-old mom of two, shared the news of her breast cancer “scare” this week and urged her fans, “Please, please ladies – get your mammograms and Pap smears! ”
Read MoreView this post on Instagram
It’s important to note that a breast biopsy, which McCain had done, is performed when a suspicious lump or calcifications are found on a physical exam or a mammogram. The procedure involves inserting a very fine needle into the suspicious area and removing a small amount of tissue to determine if it is, in fact, cancer. It’s typically a short procedure that may not be comfortable but shouldn’t be painful. There’s usually no scarring from a breast biopsy, though some patients may experience a little bruising.
RELATED: What to Expect from a Breast Biopsy
There are several different ways breast biopsies are done. Most are done using mammography to locate the tumor. Ultrasound can also be used. And if neither of these techniques work, magnetic resonance imaging (MRI) is a third option.
McCain explained further, “It is so important and vital and something I know a lot of us put off. I am 40 and this was a scare for me.
“Get your mammograms!!! Doctors, nurses, pathologists, the mammogram coordinators, all of these people are nothing short of selfless angels who walk among us and I am forever grateful to every single health care professional.”
She concluded by wishing everyone a “happy, blessed, HEALTHY New Year!”
View this post on Instagram
McCain then followed up with a celebratory New Years post, sharing footage of her and her adorable daughters counting down to the start of 2024 with party headbands and apple juice in their cups.
“We did the countdown for them at 7:00 with apple juice. Happy New Year!!” she wrote alongside the video clip.
We’re delighted to see McCain moving forward after her health scare with a drive to inform others about the importance of breast cancer screenings, especially after her beloved dad John McCain passed away from brain cancer.
Her started treatment for glioblastoma (GBM) brain cancer in July 2017, and concluded his treatment before passing in August 2018.
Having coped with grief that comes with the loss of a loved one, it’s clear McCain understands what matters most in life, as she share another uplifting Instagram post earlier this month.
She shared a list of “the real luxuries in life,” captioning the post, “Bringing this vibe with me into 2025. Love this from @thebizsecrets and couldn’t agree more.”
The list reads:
- Time
- Health
- A quiet mind
- Slow mornings
- Ability to travel
- Rest without guilt
- A good night’s sleep
- Calm and “boring days”
- Meaningful conversations
- Home-cooked meals
- People you love
- People who love you back
View this post on Instagram
How Can Gratitude Lead to a Healthier Mindset?
Gratitude: what is it and why does it matter? You’ve probably heard the word thrown around here and there when discussing complex concepts. But living with gratitude is quite simple in its meaning. It means being thankful for what you have and showing appreciation in your day to day life and it can be really helpful for those struggling with mental hardships.
Dr. Zuri Murrell, a colorectal cancer surgeon at Cedars-Sinai Medical Center, told SurvivorNet that his patients who live with gratitude tend to handle treatment better because this attitude is one way to stay mentally healthy.
Dr. Zuri Murrell On Living With Gratitude
One reason this phenomenon is often reported anecdotally could be due to the reduction in stress level. Stress and anxiety can lead to physical issues, and practicing gratitude can help get both under control.
“The patients who do well with cancer, they live life with that kind of gratitude, but in terms of everything,” he explained. “They’re grateful, not for cancer, but they’re grateful for an opportunity to know that life is finite.”
According to the National Alliance on Mental Illness, multiple studies have indicated that learning to live with gratitude can lead to more happiness and less stress. One way to exercise gratitude is to take time to think about things you appreciate everyday, and some people find it helpful to write down those things in a journal.
Helpful Information About Breast Cancer Screening
The medical community has a consensus that women between 45 and 54 have annual mammograms. However, an independent panel of experts called the U.S. Preventive Services Task Force (USPSTF) is saying that women should start getting mammograms every other year at the age of 40, suggesting that this lowered the age for breast cancer screening could save 19% more lives.
More on Breast Cancer Screening
- Bi-Annual Mammograms At Age 40 Now Recommended For Most Women, What The New Breast Cancer Screening Guidelines Mean For You
- The Mammogram Debate: Should Women Start Breast Cancer Screening at 30?
- 6 Common Excuses for Skipping a Mammogram That You Need to Stop Using!
- Mammograms Are Still the Best Tool for Detecting Breast Cancer — A Warning About Thermography
- How to Avoid False Positive Cancer Results in Women With Dense Breasts: Ultrasounds Used in Addition To Mammograms
- Black Women May Need To Start Breast Cancer Screening At 42, According To A New Study
- Breast Cancer: Introduction to Prevention & Screening
For women aged 55 and older, the American Cancer Society recommends getting a mammogram every other year. However, women in this age group who want added reassurance can still get annual mammograms.
RELATED: ‘Annual’ Screenings For Breast Cancer Survivors May Not Be Necessary, New Study Suggests
Women with a strong family history of breast cancer, have dense breasts, have a genetic mutation known to increase the risk of breast cancer, such as a BRCA gene mutation, or a medical history, including chest radiation therapy before age 30, are considered at higher risk for breast cancer.
WATCH: Understanding the BRCA gene mutation
Experiencing menstruation at an early age (before 12) or having dense breasts can also put you into a high-risk category. If you are at a higher risk for developing breast cancer, you should begin screening earlier.
Breast density is determined through mammograms. However, women with dense breasts are at a higher risk for developing breast cancer because dense breast tissue can mask potential cancer during screening. 3D mammograms, breast ultrasound, breast MRI, and molecular breast imaging are options for women with dense breasts for a more precise screening. It is important to ask your doctor about your breast density and cancer risk.
RELATED: 3D Mammography Detects 34% More Breast Cancers Than Traditional Mammography
Family History & Breast Cancer Risk
Although breast cancer can happen to anyone, certain factors can increase a person’s risk of getting the disease. The known risk factors for breast cancer include:
- Older age
- Having a gene mutation such as the BRCA1 or BRCA2
- Added exposure to estrogen
- Having children after the age of 30
- Exposure to radiation early in life
- Family history of the disease
RELATED: Is Genetic Testing Right for You?
Different types of genetic testing can help people with a family history of cancer better ascertain their cancer risks. Your doctor will discuss your family history of cancer with you in the context of your type of tumor and your age at diagnosis. Hereditary genetic testing is usually done with a blood or saliva test.
WATCH: Understanding genetic testing for breast cancer.
About ten percent of breast cancers are hereditary, says Dr. Ophira Ginsburg, Director of the High-Risk Cancer Program at NYU Langone’s Perlmutter Cancer Center.
“We encourage only those with a family history to get [genetic testing],” Dr. Ginsburg previously told SurvivorNet. “I would say that if you have anyone in your family diagnosed with a rare cancer. Or if you have a strong family history of one or two kinds of cancer, particularly breast and ovarian, but also colon, rectal, uterine, and ovarian cancer, that goes together in another cancer syndrome called the Lynch Syndrome.
The second test involves the genetic sequencing of your tumor if you’ve been diagnosed with cancer by this point. These genetic changes can be inherited, but most arise during a person’s lifetime. This process usually involves examining a biopsy or surgical specimen of your tumor. This testing can lead to decisions on drugs that might work against your cancer.
“Digital mammography, it turns out, significantly improves the quality of the mammogram… It’s 3D or tomosynthesis mammography,” Dr. Lehman explains.
“This allows us to find more cancers and significantly reduce our false-positive rate. With digital mammography 3D tomosynthesis, we’re taking thin slices through that breast tissue, like slices of a loaf of bread. We can look at each slice independently rather than trying to see through the entire thickness of the entire loaf of bread. So those thin slices help us find things that were hidden in all the multiple layers,” Dr. Lehman adds.
Additional testing can be considered for dense breasts, depending on a woman’s personal history, preferences, and her physician’s guidance.
Screening Options for Women with Dense Breasts
Women with dense breasts should get additional screening to supplement their mammograms. Dense breasts mean more fibro glandular tissue and less fatty breast tissue exists.
The dense tissue has a “masking effect on how well we can perceive cancer and find cancer on mammograms,” Dr. Cindy Ly, a radiology doctor at NYU Langone Medical Center, told SurvivorNet in an earlier interview.
Survivors Encourage Women to Ask Their Doctors About Dense Breasts
Glandular tissue within dense breasts appears white on mammograms, which can help mask potential cancer. The “frosted glass” effect from the glandular tissue can thus mask cancerous areas, especially developing ones. Undetected, these cancers can progress, growing large and advanced. They will then likely require more intensive treatments to cure or can become incurable altogether.
Women with dense breasts may not know they have it based on feeling alone. It’s important to know that breast density is determined by its appearance on a mammogram. Dr. Connie Lehman, the chief of the Breast Imaging Division at Massachusetts General Hospital, previously explained to SurvivorNet that fatty breast tissue appears gray on an X-ray. Conversely, dense breast structures appear white during an X-ray. Cancers also appear white on an X-ray, meaning the dense breast structures can mask the possibility of cancer. Luckily, advanced mammograms exist to help doctors navigate this obstacle.
WATCH: 3D Mammograms explained.
“Digital mammography, it turns out, significantly improves the quality of the mammogram…It’s 3D or tomosynthesis mammography,” Dr. Lehman explains.
“This allows us to find more cancers and to significantly reduce our false-positive rate. With digital mammography 3D tomosynthesis, we’re taking thin slices through that breast tissue, like slices of a loaf of bread. We can look at each slice independently rather than trying to see through the entire thickness of the entire loaf of bread. So those thin slices help us find things that were hidden in all the multiple layers,” Dr. Lehman adds.
Additional testing can be considered for dense breasts, depending on a woman’s personal history, preferences, and her physician’s guidance. These tests include:
- 3-D Mammogram (Breast Tomosynthesis): This technology acquires breast imaging from multiple angles and digitally combines them into a 3D representation of the breast tissue. This allows physicians to see breast tissue architecture better, even in dense breasts. 3D mammograms are fast becoming the standard way of performing mammography.
- Breast Magnetic Resonance Imaging (MRI): An MRI machine uses magnets to create highly detailed, intricate images of the breast. These are mostly reserved for women with an extremely high breast cancer risk. Dense breasts alone may not be a valid reason to obtain a breast MRI. However, dense breasts in women with genetic mutations, like BRCA1 and BRCA2, or a strong family history of breast cancer could justify obtaining breast MRIs.
- Molecular Breast Imaging (MBI): MBI is a newer imaging technique that uses a radioactive tracer to detect breast cancer. It is beneficial for women with dense breasts. However, MBI is not as widely available as other screening methods.
A new rule from the Food and Drug Administration (FDA) says that facilities offering mammograms must notify patients about their breast tissue density and recommend they speak with a doctor to determine if further screening is necessary. There will be “uniform guidance” on what language to use and what details must be shared with the patient to make the communication clear and understandable.
Breast Cancer Symptoms & Self-Exams
Women are encouraged to do regular self-exams to become familiar with how their breasts feel normally so something like a lump forming can be easily detected. A self-exam includes pressing your fingertips along your breast in a circular motion.
If you feel something abnormal, such as a lump or discharge from the nipple, you should contact your doctor for further examination.
Below are common symptoms to look out for:
- New lump in the breast or underarm (armpit)
- Any change in the size or the shape of the breast
- Swelling on all or part of the breast
- Skin dimpling or peeling
- Breast or nipple pain
- Nipple turning inward
- Redness or scaliness of breast or nipple skin
- Nipple discharge (not associated with breastfeeding)
Learn Your Risk and Listen to the Guidelines: An Important Message About Breast Cancer Awareness
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

