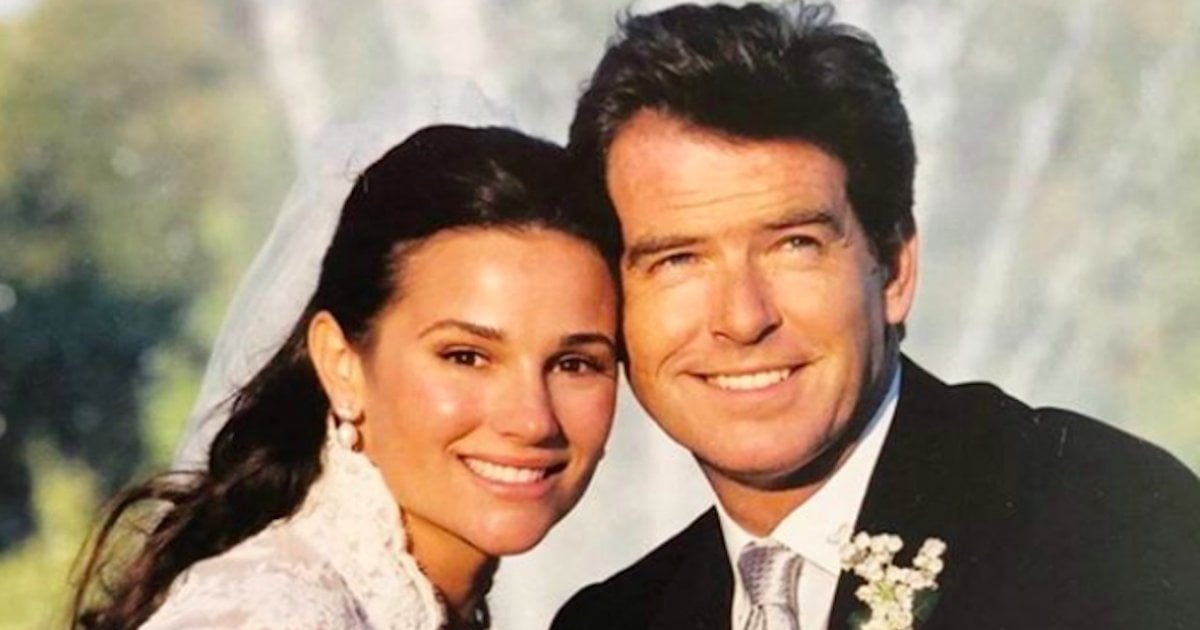
Doting family man, Pierce Brosnan, is celebrating the healing milestone that soothed his profound grief after his first wife, Cassandra Harris, lost her battle with ovarian cancer in 1991 at age 43. “Happy anniversary my love Keely…my brown-eyed girl,” the former James Bond actor shared on Instagram. “Should I fall behind wait for me…as ever, my love.”
Read MoreView this post on Instagram
They have two sons, Dylan, 23, and Paris, 19. Brosnan and Cassandra’s son, Sean Brosnan, 36, was just eight years old when his mother died.
"You are the finest, loveliest, and tenderest person I have ever known,” she responded. “🥂 Happy Anniversary”
Pierce Brosnan's Lost Loves: Ovarian Cancer
Brosnan has credited his wife of 19 years, Keely Shaye Smith Brosnan, with helping him find his way through his grief after ovarian cancer took the lives of his first wife, Cassandra, her mother, and her daughter, Charlotte who died at 41.
Brosnan adopted Charlotte after her own father's death and the actor considered her one of his own.
The signs of ovarian cancer can include feeling bloated or full, pain in the pelvis or abdomen, nausea, vomiting, or changes in bowel habits, says Dr. Jose Alejandro Rauh-Hain, a gynecologic oncologist at MD Anderson Cancer Center.
"From day one, we really had a fight on our hands," Brosnan said of Cassandra's disease in an interview with PEOPLE a year after her death. "This wasn't a shadow or a small tumor this had invaded Cassie's being." Over four years, Cassandra endured eight surgeries and a year and a half of chemo.
"I never asked Cassie if she was scared. I regret that," Brosnan told PEOPLE. "I didn't want to ask, because she had so much fight." But there were times, he says, when she would say, "I need you," and those moments "cut like a knife."
As Cassie's life neared the end, Brosnan said, "She was comforting me. She said, 'Please, darling, don't worry. It's just a life winding down' … up until then there was always something, some new treatment. But then the options got fewer and fewer."
The Cancer That Whispers
Ovarian cancer is often referred to as the "cancer that whispers," says Dr. Beth Karlan, Director of the Women's Cancer Program at the Cedars-Sinai Medical Center. It has symptoms that are very vague and often mimic the ordinary discomforts associated with a woman's menstrual cycle or menopause. However, if you are experiencing any of the following symptoms, and they seem to be getting worse, it is worth it to see a doctor to rule out ovarian cancer:
- Feeling full earlier/decrease in appetite
- Feeling bloated
- Changes in bowel habits
- Pain in the pelvis
- Urinary symptoms, such as an urgent need to go
- Extreme fatigue
- Abdominal swelling
- Pain during sex
Roughly half of the women diagnosed with ovarian cancer are over age 60. Because of this, many doctors will write off symptoms as signs of menopause. Since there is no screening test for ovarian cancer so far, only about 20% of cases are diagnosed in the early stages, according to the American Cancer Society.
Dr. Beth Karlan, a gynecologic oncologist at UCLA Medical Center on screening for ovarian cancer
In a conversation with SurvivorNet, Dr. Karlan also pointed out the average delay from the time a woman notices symptoms to the time that she is diagnosed with ovarian cancer is around 9 months.
"That's why, if you do have these symptoms, even if it's only for two weeks but they're happening everyday and seem to be getting worse, you should call your doctor and say, 'I'm having these symptoms. I'm concerned it could be ovarian cancer. Can I have an ultrasound and a CA-125,'" Dr. Karlan said.
Genetic Testing For Ovarian Cancer
Even though ovarian cancer impacts women, genetic testing can benefit men as well. Genetic defects associated with ovarian cancer are autosomal dominant which means they can be carried in both men and women. Men can also inherit a BRCA-1 or BRCA-2 mutation and an increased risk for certain cancers.
RELATED VIDEO: What is a BRCA Mutation?
Men with BRCA mutations have a higher-than-average lifetime risk for developing breast and prostate cancer. Their children have a 50 percent chance of carrying the same gene mutation, and the associated cancer risk.
Dr. Oliver Dorigo, a Gynecologic Oncologist at Stanford Medical School, says advances in ovarian cancer have led to improved patient survival rates.
For families devastated by ovarian cancer, the question of genetics often weighs heavily on survivors wondering if children or grandchildren have face a higher risk of developing the disease. But genetic testing results can also guide crucial treatment decisions.
RELATED: Two Major New Ovarian Cancer Approvals Expanding Access To PARP Inhibitors
At least 10 to 15 percent of ovarian cancers are based on inherited (or germline) mutations, says Dr. Irina Dimitrova, gynecologic oncologist at Henry Ford Health System in Detroit. Mutations of the BRCA gene place women at a heightened risk for both ovarian and breast cancer as well as pancreatic or colon cancer, says Dimitrova. In the U.S., 90 percent of people who carry a BRCA gene mutation aren't aware of it until someone in their family gets cancer.
Dr. Beth Karlan, a gynecologic oncologist at UCLA Medical Center did not treat Cassandra or Charlotte, but advises genetic testing can have life-saving benefits, especially because ovarian cancer is curable in over 90 percent of cases when diagnosed early on.
"It's important when you're deciding whether or not genetic testing would benefit you to try to find out what types of things run in your family," Dr. Karlan says. "Because it can really help to save lives."
Learn more about SurvivorNet's rigorous medical review process.