Survivorship After Colon Cancer
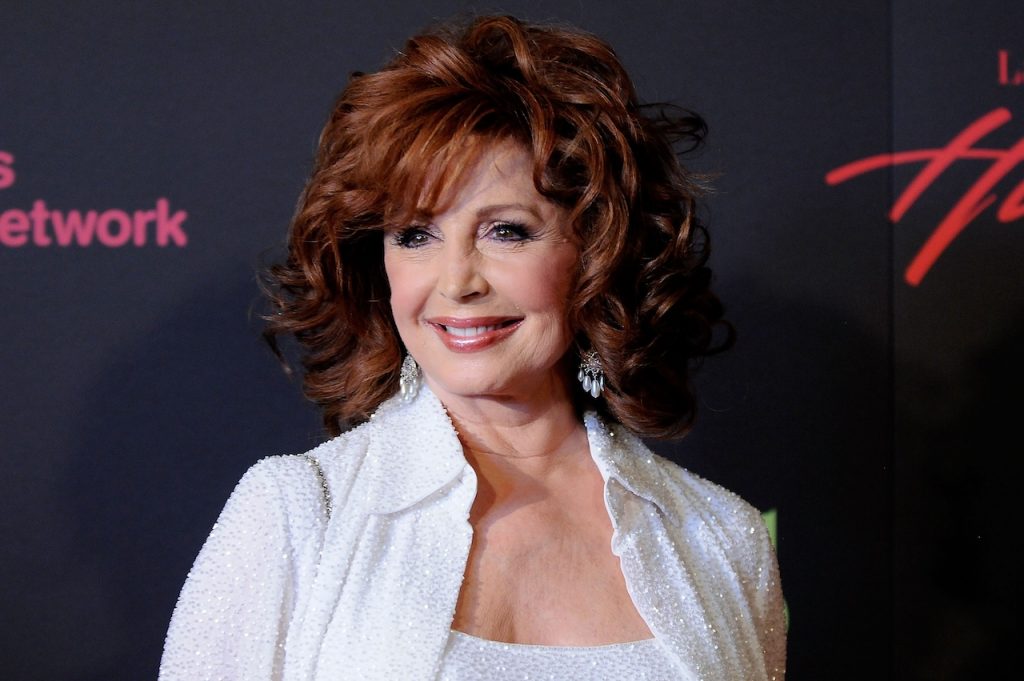
- Suzanne Rogers, 82, “Days of Our Lives” longest-serving actress, is in remission from stage 2 colon cancer and grateful for a renewed outlook on life after surgery, chemotherapy, and radiation treatment.
- Colonoscopies are the most effective way to screen for colon cancer, according to SurvivorNet experts, and they’re important for both prevention and early detection.
- If you’re at average risk for this type of cancer, meaning you don’t have risk factors like smoking or a family history of the disease, the American Cancer Society advises getting regular colonoscopies once you turn 45, and as early as 35 if you do have a heightened risk.
- It’s important to remember that once patients reach survivorship, as Rogers recently did, this period isn’t just an end state – it’s a continuous journey. It begins the moment a person is diagnosed with a significant health condition and continues throughout their life. You might hear people say things like, “from the moment of diagnosis, you become a survivor.”
Speaking at Peacock’s Days of our Lives 60th Anniversary Celebration, Rogers told People that she’s now in remission and embracing life with a renewed perspective.
Read MoreView this post on Instagram
Rogers, whose stage name was inspired by the late actress and dancer Ginger Rogers, then opened up about her approach to life, explaining, “I don’t worry about the small things. It’s not worth it.”
“I was rushing here, and I went, ‘Wait a minute. You’re not going anywhere.”
She also credited her family and faith for guiding her through her challenging health journey.
Rogers, who admitted she’s regaining her strength slowly and is “about 70%” recovered, recounted, “The day before I started my chemo and radiation, my priest, I told him, I said, ‘Can I talk to you about something?’ I said, ‘I’m starting chemo and radiation tomorrow.’ He said, ‘Come with me.’ And he took me into the church, up the aisle, up on the altar.
“He said, ‘Stand right here.’ And he went and got some oils and a prayer and did the anointing. So I felt that that’s what helped me through.”
Roger’s health news comes after she took a leave of absence in her fight against colon cancer.
She recently told TV Insider that she underwent cancer treatment every day for six weeks, which included both chemotherapy and radiation therapy. She began treatment on June 16 and concluded it on July 31.
View this post on Instagram
Rogers remembered first feeling “off” over the summer, which prompted her to visit her doctor. After having a colonoscopy done, an exam she had done regularly, a surgeon advised her to get an MRI, a PET scan, and a biopsy.
Following the additional testing, Rogers recalls her doctor telling her, “You have cancer and you have to start treatment,” something which came as a shock to her.”
She added, “I think I was in shock for several days because I take pretty good care of myself. But he [the doctor] said, ‘It’s a good thing you caught it in time.'”
The regular six-week hiatus in the “Days of Our Lives” filming schedule, over the summer, allowed Rogers to keep her diagnosis private.
“I was able to keep it under wraps, and then the show took that break, so it wasn’t necessary to get into it all then. It helped me because it gave me even more time to chill and to get myself healthy,” she said.
Rogers, with no intention of leaving the show, pointed out that audiences won’t see her absence until 2026, as the series films episodes almost a year ahead of their air date.
Understanding Colon Cancer
Colorectal cancer happens when polyps are not removed and become cancerous. It can take up to 10 years for a colon polyp to become cancerous, according to SurvivorNet experts.
“We know that colon cancers can be prevented when polyps are found early,” Dr. Heather Yeo, a surgical oncologist who specializes in colorectal cancers at Weill Cornell Medicine, told SurvivorNet.
“Lowering the screening age helps somewhat with this, but access to care is a real problem,” Dr. Yeo added.
Dr. Zuri Murrell, a colorectal cancer surgeon and Director of the Cedars-Sinai Colorectal Cancer Center, previously explained the colonoscopy procedure to SurvivorNet.
Expert Colon Cancer Resources
- All Americans Should Begin Colorectal Cancer Screening at Age 45, According to New Guidelines; Previous Age Was 50
- Colon Cancer Screening Options And Genetics: Myth Busting With Dr. Heather Yeo
- FDA Approves Blood Test for Colon Cancer Screening — What This Means for Patients
- Clinical Trials for Colorectal Cancer Can Offer Cutting-Edge Treatment
- Debating Over Treatment of Colorectal Cancer – The New Evidence About Watch and Wait
- Colorectal Cancer Is On The Rise in Young Adults — Here’s What We Know
- Colorectal Cancer Screening: a New Study Questions the Effectiveness of Colonoscopies But Specialists Reinforce its Importance
“When we see a polyp, we actually physically take the polyp out through the colonoscope,” he explained. “What does that mean? That means we basically put a wire through with a little bit of a flange at the end, and we pull the polyp out. Now, note there is no pain with that. Inside the colon, there are no pain fibers. So, there’s no pain.”
The advantage of a colonoscopy is that your doctor can remove any polyps found during the test. Many colon cancers can be caught on a colonoscopy before they develop or when the polyps are small enough to be removed without surgery.
Looking for Polyps During Colonoscopy
The American Gastrointestinal Association lowered the recommended initial age for a colorectal screening from 50 to 45.
The U.S. Preventive Services Task Force recommends guidelines that state colon cancer screenings should begin at 45 years old. This is in response to the increase we see in colon cancer diagnoses in younger adults.
However, many insurance companies still do not cover the cost of screenings for those under 50. In the past, the disease had predominantly been found in adults 50 years or older, but for those predisposed to getting it at a younger age, these new guidelines could help catch it earlier.
Colon Cancer: A Silent Killer
Dr. Heather Yeo, a colorectal surgeon and surgical oncologist at Weill Cornell Medicine and New York-Presbyterian, previously told SurvivorNet, “Colon cancer is considered a silent and deadly killer.
RELATED: How Does a Colon Polyp Turn Into Cancer?
“What happens is people often don’t know that they have colon cancer. They don’t have any symptoms. That’s why we screen for colon cancer in the United States.”
The Rate of Colon Cancer is Increasing in Those Under 50
“You should be screened for colon cancer, even if you have no family history. Once you have your initial screening colonoscopy, if there are no polyps and you have no high-risk factors, usually once every 10 years is fine,” she advises.
“Colon cancer is a slowly progressing cancer. If you have any family history of colon cancer, you should be screened about 10 years before a family member had colon cancer. So if you have a family member who was 53, you should be screened at 43.”
Dr. Paul Oberstein Explains Common Colon Cancer Symptoms
What Increases Your Risk for Developing Colon Cancer?
For some people, certain risk factors can influence their risk of getting colon cancer. They include the following:
- Are older. About 90% of cases are in people aged 50 or older, according to the U.S. Centers for Disease Control & Prevention (CDC). Yet it is possible to get this cancer earlier in life.
- Have inflammatory bowel disease. Crohn’s disease or ulcerative colitis can, over time, cause cells in your intestines to turn cancerous.
- Have a family history of this cancer. Just under one-third of people who get colon cancer have family members with the disease.
- Have a gene mutation. About 5% of colorectal cancers are caused by an inherited genetic mutation that causes syndromes such as familial adenomatous polyposis (FAP) or hereditary nonpolyposis colorectal cancer (Lynch syndrome).
- Don’t exercise very often. Staying active can lower your risk.
- Eat a diet that’s high in meat. Regularly eating red meats like burgers and steaks, and processed meats such as hot dogs and bacon, might put you at a higher risk. Eating more fruits, vegetables, and whole grains instead might lower your risk.
- You are overweight or obese. Having too much weight increases your risk of both getting colon cancer and dying from it.
- Drink a lot of alcohol. Limiting alcohol to one drink daily for women and two drinks daily for men could help lower your risk.
- Use tobacco. Long-term smokers are more likely to get this cancer than nonsmokers.
Which Treatments are Best for You?
It’s important to understand that your doctor has many ways to treat colon cancer, depending on what stage the cancer is, including:
- Surgery
- Radiation therapy
- Chemotherapy
- Targeted therapy
- Immunotherapy
Surgery
Surgery is the main treatment for most early-stage colon cancers, according to the doctors SurvivorNet spoke with. The surgeon will remove the part of the colon or rectum where there is cancer, along with a small area of healthy tissue around it. Taking out as much of the cancer as possible is important for improving your outcome.
The surgery may be performed through small incisions (laparoscopy) or through a larger incision. Some people may need to wear a special bag (ostomy) to collect waste after surgery.
Radiation Therapy
This treatment aims high-energy X-rays at the cancer to destroy the abnormal cells. The radiation can come from a machine outside your body or be placed directly inside your body. Sometimes people get radiation before surgery to shrink the tumor and make it easier for the surgeon to remove. This is called neoadjuvant radiation.
Chemotherapy
This treatment uses strong medicine to stop cancer cells from dividing, no matter where they are in your body. You may get a combination of chemotherapy drugs as your first treatment. Chemotherapy has been very well studied for colorectal cancer, and it is known to improve survival.
The most common therapy is a combination of chemo drugs called FOLFOX:
- FOL = leucovorin calcium (folinic acid)
- F = fluorouracil
- OX = oxaliplatin
Your doctor may add medications like irinotecan (FOLFIRI) or cetuximab, depending on how well your tumor shrinks with treatment and other specifics about your particular cancer. For FOLFOX, the medications are given through the vein and require regular doctor visits.
To determine exactly which chemotherapy regimen you get, your doctor will consider your age and how well you might tolerate the side effects of chemotherapy. Gene mutations (for example, BRAF and KRAS) and the location of the primary colon tumor also factor into the decision.
You can also get chemotherapy before colon cancer surgery, which is called neoadjuvant chemotherapy. Getting chemo first helps to shrink the tumor, which can make both the surgery and recovery easier, according to SurvivorNet’s experts. Chemo is also a treatment for cancer that returns after therapy.
Targeted Therapy
This treatment targets substances like proteins or genes that the cancer needs to grow. This makes targeted therapy more precise than chemotherapy and less likely to damage healthy cells. One example of targeted therapy is bevacizumab (Avastin), which stops the growth of new blood vessels that feed tumors. Another group of targeted therapies is called epidermal growth factor receptor (EGFR) inhibitors, which block the cancer from growing.
Immunotherapy
This treatment makes your own immune system a more efficient cancer fighter. A group of drugs called checkpoint inhibitors, which includes pembrolizumab (Keytruda) and nivolumab (Opdivo), work by preventing cancer cells from hiding from your immune system. Checkpoint inhibitors may extend the amount of time before the cancer spreads.
Dr. Paul Oberstein discusses the treatments doctors use to turn stage 4 colon cancer into a chronic but manageable disease
What You Need to Know About Survivorship
Whether you’re beginning your journey into survivorship or are a seasoned survivor, you’ll quickly learn that it’s a term with many layers. At its simplest, ‘survivorship’ signifies the state of living beyond a challenging event or diagnosis, such as cancer. More specifically, it marks the period after treatment where a patient goes from merely surviving to thriving, as they navigate their newfound lease on life.
It’s important to remember that survivorship isn’t just an end state – it’s a continuous journey. It begins the moment a person is diagnosed with a significant health condition and continues throughout their life. You might hear people say things like, “from the moment of diagnosis, you become a survivor.”
It’s a powerful sentiment that reflects the courage and resilience involved in battling a serious illness.
Being a survivor also means redefining your life while coping with the aftermath of disease and its treatment. This phase might include the challenge of dealing with physical and emotional changes, attending regular check-ups, the fear of recurrence, or the need for long-term medication. Despite these hurdles, many survivors find unique strength, growth, and transformation during this time.
Survivorship is much more than just the absence of disease—it’s a new stage of life, a rite of passage. Your journey might not have been one you would have chosen, but through it, you’ll uncover a greater understanding of yourself and what you’re capable of. Each person’s survivorship journey is unique, and how you choose to travel is entirely up to you.
Remember—navigating this new terrain called ‘Survivorship’. It might be challenging, but remember, you’re not alone. There are ample resources and support systems designed to help you along the way.
Continued Medical Care
Don’t lose sight of the importance of continued medical care – always keep your follow-up appointments and adhere to any healthcare recommendations.
Remember, embracing these coping strategies can help you navigate your way into survivorship with greater ease and renewed energy. Just remember – slow and steady wins the race! You’ve overcome huge hurdles; it’s okay to take this new stage of your life at your own pace.
Resilient learning to overcome any obstacle
Additionally, health checkups are an integral part of maintaining wellness and spotting potential health issues early. This holds true for everyone, but even more so for a person who’s in the throes of survivorship.
One of the main reasons you’ll want to maintain routine health checks is to monitor for recurrence. While the hope is always for complete recovery, there’s a possibility of the disease returning—even with successful treatment. Regular checkups allow you to keep a vigilant eye on the situation, leading to early detection and treatment if any problem emerges.
Managing Other Health Conditions & Healthy Lifestyle Changes, Matters Too!
A survivorship journey can occasionally lead to new health conditions, including heart problems, diabetes, or osteoporosis. Routine screenings and monitoring help keep these conditions under control, ensuring they don’t escalate into major health risks.
Regular checkups also serve as an opportunity for your health care provider to give advice on healthy lifestyle changes. This includes exercise, a balanced diet, stress management, and quitting habits like smoking and excessive alcohol consumption—factors that can significantly lower the risk of recurrence or other health issues.
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.

