The Power of CAR T-Cell Therapy
- CAR T-Cell Therapy is a personalized type of immunotherapy that trains your own immune system to fight cancer. While T-cells—your body’s natural defenders—normally seek out and destroy abnormal cells, cancer can learn to “hide,” making it harder for those cells to be detected and attacked by the disease.
- Dr. Premal Lulla, at Baylor College of Medicine, describes CAR T-Cell Therapy with a metaphor: “It’s like an army and a navy and the entire battalion comes to the tumor site to eliminate the tumor.”
- Understand the Commitment and Risks: While CAR T-Cell Therapy has a lot of promise for patients with diffuse large B-cell lymphoma, patients should be aware of the manufacturing timeline, costs and potential side effects.
- Goal of Treatment: For diffuse large B-cell lymphoma patients, CAR T-Cell Therapy offers a potential path to cure.
A Breakthrough Option for Diffuse Large B-Cell Lymphoma Patients in Houston
CAR-T Cell Therapy has shown remarkable success in treating diffuse large B-cell lymphoma—the most common type of non-Hodgkin lymphoma—helping many patients achieve long-lasting remission even after other therapies have stopped working.Diffuse large B-cell lymphoma patients in the Houston region may have an easier path to CAR T-Cell Therapy, as the area is home to a multitude of specially certified centers equipped with the infrastructure and trained staff to administer CAR T-Cell Therapy.
Read MoreWhat Is CAR T-Cell Therapy?
Dr. Premal Lulla, a medical oncologist at Baylor College of Medicine, describes CAR T-Cell Therapy with a metaphor: “It’s like an army and a navy and the entire battalion comes to the tumor site to eliminate the tumor.” CAR T-Cell Therapy is a form of personalized immunotherapy — a treatment designed to use your body’s own immune system to fight cancer. Normally, your immune system relies on T-Cells (a type of white blood cell) to detect and destroy abnormal or infected cells. But cancer cells can learn how to “hide” from these T-Cells, making it harder for your immune system to recognize and attack them.CAR T-Cell Therapy overcomes this problem by reprogramming your own T-Cells to better identify and destroy cancer cells.
Here’s how the process works, step by step:
- T-Cell Collection (Leukapheresis) – Doctors collect some of your T-Cells from your blood. This is done through a special procedure called leukapheresis, which separates white blood cells from your blood and returns the rest to your body. The process usually takes a few hours and is not painful.
- Genetic Engineering in the Lab – In a laboratory, your T-Cells are modified to add a new gene that makes a special receptor called a Chimeric Antigen Receptor (CAR). This CAR acts like a “homing device,” helping your T-Cells recognize a specific marker (antigen) found on your cancer cells — for example, CD19 on B-cell lymphomas or leukemias.
- Expansion and Preparation – Once engineered, the CAR T-Cells are grown and multiplied until there are millions of them — enough to effectively fight the cancer.
- Reinfusion into the Patient – After a few weeks, the modified CAR T-Cells are returned to you through an IV infusion. Before this step, you’ll get a short round of chemotherapy to help your immune system make space for the new cells to work.
Once infused, the CAR T-Cells circulate through your bloodstream, recognize cancer cells, and mount a powerful immune attack. Some of these CAR T-Cells remain in your body as “memory cells,” continuing to guard the body against cancer cells long after treatment ends.
WATCH: CAR T-Cell Therapy As A Cure
Doctors carefully evaluate whether CAR T-Cell Therapy is appropriate for each person. Eligibility depends on factors such as:
- Type and stage of cancer
- Previous treatments and how well you tolerated them
- Overall health and organ function
- Ability to undergo hospitalization and close monitoring
Despite the risks, Dr. Lulla emphasizes, “you want to give every patient who has failed combination chemotherapy an opportunity to get CAR T-Cells because you know that it is probably going to cure many of these patients.” Because CAR T-Cell Therapy can cause strong immune reactions, it’s generally offered in specialized centers with experience managing these side effects.
If you’re interested in CAR T-Cell Therapy, your oncologist may refer you to a treatment center that performs these therapies or discuss whether you’re eligible for a clinical trial exploring newer CAR T-Cell Therapy designs or cancer types.
How Is the Treatment Delivered?
CAR T-Cell Therapy involves several key steps spread out over a few weeks:
- Consultation and Evaluation – You’ll meet with the CAR T-Cell Therapy team (oncologists, nurses, and specialists) to review your medical history and confirm eligibility.
- T-Cell Collection (Leukapheresis) – Your T-Cells are collected through a machine that filters your blood.
- Manufacturing Period – Your cells are sent to a lab for engineering. This step can take 2–4 weeks, depending on the product.
- Bridging Therapy (if needed) – If your cancer is growing quickly, your doctor may give temporary chemotherapy while waiting for your CAR T-Cells to be ready.
- Lymphodepleting Chemotherapy – A short, low-dose chemotherapy regimen (usually 3 days) helps prepare your immune system.
- CAR T-Cell Infusion – The modified cells are given back through an IV, usually in the hospital. The infusion itself takes less than an hour, but you’ll be monitored closely afterward.
After the infusion, you’ll remain in the hospital for at least 1 to 2 weeks so your care team can monitor you for early side effects and address them promptly. Following this, you’ll have regular follow-up visits over the next several weeks or months.
Expert Resources on Non Hodgkin Lymphoma
- From Discovery to Breakthrough: The Scientific Journey Behind CAR T-Cell Therapy
- CAR T-Cell Therapy: Hope, Hurdles, and What to Expect
- CAR T-Cell Therapy Side Effects Can Be Serious, But Many Are Short-Lived
- CAR T-Cell Therapy for Non-Hodgkin Lymphoma
- CAR T-Cell Therapy, Bispecific Antibodies — Choosing Between Innovative Treatment Options
- CAR T-Cell Therapy: A Step-By-Step Guide to Having This Breakthrough Treatment
What Are My Chances of a Cure with CAR T-Cell Therapy?
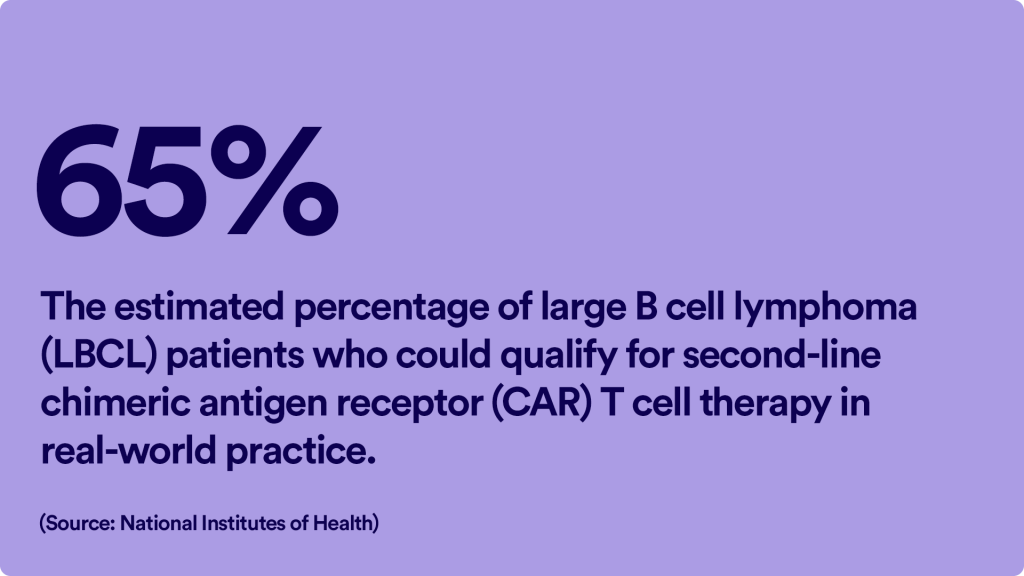
CAR T-Cell Therapy has produced remarkable results, especially in patients whose cancers had stopped responding to other treatments. While not every patient is cured, many have achieved complete remission. Around 40–50% of B-cell lymphoma patients achieve long-term remission
Because CAR T-Cell therapy is still relatively new, researchers are continuing to study how long remissions last and whether some patients can be truly cured.
Even when a cure isn’t possible, CAR T-Cell Therapy can significantly improve quality of life, reduce symptoms, and provide patients more time with loved ones.
Living Beyond CAR T-Cell Therapy
If you respond to CAR T-Cell Therapy, you’ll have regular follow-up visits for months or even years to keep your immune system healthy and to watch for any signs of recurrence. Many patients are able to gradually resume normal daily activities within a few months.
Learn more about SurvivorNet's rigorous medical review process.